energyandstruct
Member
- Joined
- Nov 27, 2017
- Messages
- 960
Follow along with the video below to see how to install our site as a web app on your home screen.
Note: This feature may not be available in some browsers.
Click Here if you want to upgrade your account
If you were able to post but cannot do so now, send an email to admin at raypeatforum dot com and include your username and we will fix that right up for you.
would you say to watch out for these things as one applies the approach to raising metabolism to heal from cfs? thyroid has occasionally raised blood pressure but I think it was somewhat temporary and I don't want to get thrown into metabolic syndrome. a couple times I had to chug juice cause of how feverish and weak I felt from thyroid and I wonder if this was like temporarily induced diabetesThat's what happened to me. It has been like a pendulum swinging in the opposite direction that is just recently starting to stabilize. I never imagined how much time it would take. @aguilaroja described it once in a thread a long time ago that I'd love to find again because it helped me understand what I have been experiencing as just part of the healing process.
Some of my experience above was probably related to extreme family and work stress. I also think I persisted too long in eating some foods that didn't agree with me just because I didn't want to be orthorexic.would you say to watch out for these things as one applies the approach to raising metabolism to heal from cfs? thyroid has occasionally raised blood pressure but I think it was somewhat temporary and I don't want to get thrown into metabolic syndrome. a couple times I had to chug juice cause of how feverish and weak I felt from thyroid and I wonder if this was like temporarily induced diabetes
I must clarify this statement. I'm not recommending people stop any medication prescribed by their physician/medical team without consulting with them first. I'm only referring to substances being used to boost metabolism that aren't part of medical treatment. I've found it beneficial to stop everything several times over the years as my health has improved to see what I actually need to continue and what is no longer necessary.believe patience and perseverance are necessary but if you notice a trend over weeks or months of feeling worse I'd recommend taking a break from supplements and meds altogether and regrouping.
Dear Sheila, my temps have been about 98 on waking (up to 0.5 degree lower if I sleep poorly and not enough) and over 99 during the day. But if I overexercise, I soon begin to feel cold. I don' have data but I am sure my temperature internally drops as my inability to keep warm becomes rather intense. It rarely happens these days, but usually, before this sense of going down, I feel hungry and I always drink OJ and eat something salty.Dear Mr DesertRat
You appear to be a high temperature version of Rattus Experimentus that is to be found extensively on this forum. Greetings to you and welcome.
I am interested in your 3 years of doing thyroid...excellent temps and pulse and the 'absolutely no difference whatsoever in exercise tolerance; indeed it has gotten worse" because I have found similar in some afflicted by CFS and am ever am focused on what might be 'missing'.
This really is a punt, but I wonder if exercise triggers hypoglycaemia more readily for some reason in these people and from there symptoms seem to recur as a protective mechanism against endotoxin ingress and mitochondrial poisoning thereupon. Is cellular memory involved and how do you program the body not to panic and shut down?
Once again I don't have a very clear question here, I have just seen an improvement in some CFS people with metabolic strategies but if they go anywhere near 'overdoing' things, they're suddenly shot. Many of them have long periods without food and much physical/mental strain in their past history which would suggest considerable endotoxin damage and that there has been a strong use of cortisol to cope - as I always say, I have not met a CFS who was a 'slacker', usually quite the opposite. And their frustration with themselves at suddenly falling in a hole again is very real and tragic to observe.
If you have any thoughts, and indeed data on what your temps and pulse do on exercise, I would be pleased to hear them, thank you.
Sincerely
SheilaOceaniaRattus
interesting, im surprised how insightful he is with regard to neurotransmitters, etc, ive only read a few of his pieces on culture and narcissism and always thought he was kind of a hackDear Mr DesertRat,
Thank you for coming back to me after all this time, your responses were most interesting. I am going to trial the 'intermittent resting' with the person I have been thinking of who has such a continuously high pulse (120 resting) despite showing slow but cumulative improvement. Certainly there is also a heap of environmental toxins (pesticides) in her environment but pretty sure in her case, no mould.
The Last Psychiatrist had an interesting post which mentioned Benadryl. The Last Psychiatrist: Treating Insomnia With Less He has an interesting style of writing and alas posts no more as he was 'outed' - his day job is as a clinical psychiatrist. But anyway, here is the extract on Benadryl that you might find interesting from that blog:
"I tried antihistamines like Benadryl, and they don't work. In fact, they make me feel wired.
Ah, many people have this reaction. You'd be surprised to learn that this is due to, and a screen for, very low levels of testosterone.
What?!
Psyche.
The real reason is that it isn't actually an antihistamine. That's misleading.
What do you mean, misleading?
You know how I hate the FDA, and most everyone else in the world, because they use words to distort the truth, and get girls to sleep with them that would never sleep with me?
What?!
Pay attention.
Here is the affinity chart for Benadryl:
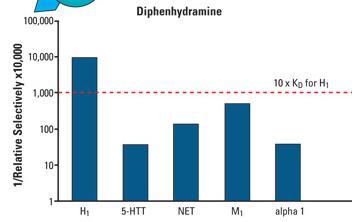
(from CNS Spectrums)
The drug has the most affinity for H1 receptors, sure, but look what else it does. M1 blockade (dry mouth, constipation, confusion.) It also has significant NE and serotonin reuptake blockade. Basically, the FDA decided to pick only one of these four properties and slap it on the box, in the same way as labeling a TV dinner as "Rice."
You'll also observe that it looks like it works the same way as Effexor or a tricyclic. You'd be right. Think about that.
So every time I take Benadryl, it's an antidepressant?
Depends on the dose.

If you eat all of this TV DINNER, you'll be getting several foods. But if you only take one single fork of the rice, then the only thing you ate was rice, even though the box says, "TV DINNER."
If you only take a low dose of Benadryl, then you are only getting H1 blockade. If you take a medium dose, then you are eating only the rice (H1 blockade) and the cogentin (M1 blockade.) A high dose gets you all of the TV DINNER and receptors blocked (and also a heart attack-- hey, the analogy holds!)
If you imagine that the drug prefers H1>M1>NET>a1>5HTT, then you see that the mistake most people make with Benadryl is that they increase the dose when if doesn't work. What you really want to do is decrease the dose, to get away from all the other things that could be stimulating (serotonin, NE, anticholinergic.)
-------------------------------------------------------------------------------------------------------------------
I hope that is useful to you. And, thinking about it, if you have any insights on elevated resting pulse I would be most interested. The standard suggestions here just don't cut it for this person, but permanent low level attack by pesticides might be enough to prevent the stress response from really turning off. This person lives in an area of intensive agricultural production.
I wish you continuing progress, all the best
Sheila
and other posts on ME-CFS poor tolerance for carbs, I found in my experience that the only fuel pathway working decently was burning aminos so I had to eat a lot of protein and always had high ammonia, which ends up negating the improved energy from burning aminos. But I found that over time, adding simple carbs like OJ and white sugar at first made me very relaxed and tired and actually too tired to even walk a block: in other words, they made the CFS feel like it was worse.
That's a good sign but be careful with fats -- you probably are avoiding PUFA if you're on this forum -- because fat metabolism can increase oxidative stress (ROS). Usually something is going on with the liver in CFS, as nearly everyone tested as exceedingly high phase 1 clearance and something incommensurate with phase 2 or 3 pathways, and phase 1 often raises the toxicity temporarily of whatever the liver is trying to clear so it can create more of a backlog. I guess what I'm saying is make sure you are supporting good liver clearance as you increase fat. For me, fruit and fruit juice really helps a lot, coffee of course, and I also do coffee enemas if I feel the need (like headache comes on)Lately, I have increased fat intake and it seems to make me feel more relaxed. I have started to see drowsiness as a good sign that I have my hormones in check.
That's a good sign but be careful with fats -- you probably are avoiding PUFA if you're on this forum -- because fat metabolism can increase oxidative stress (ROS). Usually something is going on with the liver in CFS, as nearly everyone tested as exceedingly high phase 1 clearance and something incommensurate with phase 2 or 3 pathways,
They're just a way that Functional Medicine testing categorizes steps in the activities of the liver. I think it's somewhat artificial in that there are not three distinct phases, but some things take place before others, and the categorization is helpful in determining where deficits or excesses might be.What's this about phases?
They're just a way that Functional Medicine testing categorizes steps in the activities of the liver. I think it's somewhat artificial in that there are not three distinct phases, but some things take place before others, and the categorization is helpful in determining where deficits or excesses might be.
 , increased levels of nitric oxide, regulatory T cell responses with increased levels of transforming growth factor-ß and interleukin-10, and viral/bacterial-mediated pathways [1]. Oxidative stress and energy metabolism have been elucidated as a dysfunction in the metabolic pathways of CFS patients [94]. Moreover, the response of CFS patients to accumulative exercise is related with accentuated oxidative stress, as well as with noticeable changes in the muscle membrane dysfunction that induce post-exercise malaise and muscle pain reported by CFS patients [95,96]. Finally, IgM-associated immune responses, directed against disrupted lipid membrane components and proteins, could be induced by nitrosative or oxidative stress in CFS patients [97]."
, increased levels of nitric oxide, regulatory T cell responses with increased levels of transforming growth factor-ß and interleukin-10, and viral/bacterial-mediated pathways [1]. Oxidative stress and energy metabolism have been elucidated as a dysfunction in the metabolic pathways of CFS patients [94]. Moreover, the response of CFS patients to accumulative exercise is related with accentuated oxidative stress, as well as with noticeable changes in the muscle membrane dysfunction that induce post-exercise malaise and muscle pain reported by CFS patients [95,96]. Finally, IgM-associated immune responses, directed against disrupted lipid membrane components and proteins, could be induced by nitrosative or oxidative stress in CFS patients [97]."they’ve done experiments in rabbits, taking a piece of foreign cartilage (like, from a cow) and it will produce very few antibodies in the rabitt. But if you twist it a little bit, structurally damage it, then it produces a terrific immune reaction. And any organ that gets strained or overworked tends to leak some of its proteins, and the immune system’s function, largely, is to clean up any mess. In fact, there’s an alternative interpretation of what the immune system is doing: rather than looking for foreign invading pathogens, this theory says it’s primarily cleaning up messes caused by anything which is pathogenic.