Does anyone have any idea why this could be happening?
It seemingly spontaneously started happening when I was going pretty heavy on High vitamin K doses and also on high histamine foods (bone broth, gelatin, kefir, dark chocolate) but I have since stopped eating gelatin, bone broth, dark chocolate and kefir I was having up until very recently but have cut that out too since it's gassy and makes me burp which makes the likelihood of it getting trapped more likely. I remember switching from blueberry juice to apple juice for my gelatin gummies and that's when I really started to notice it happening. Since then the belching has decreased in frequency and strength (the belches are smaller) but the issue with this is it seems like they can sometimes get stuck in my esophagus/chest
The worst part about it is the air sometimes gets stuck in my esophagus/chest and it feels like I cannot breathe properly. This activates anxiety and I start manually breathing with the constant air hunger feeling. The belches can sometimes be very very small, like 20% the size of a regular belch.
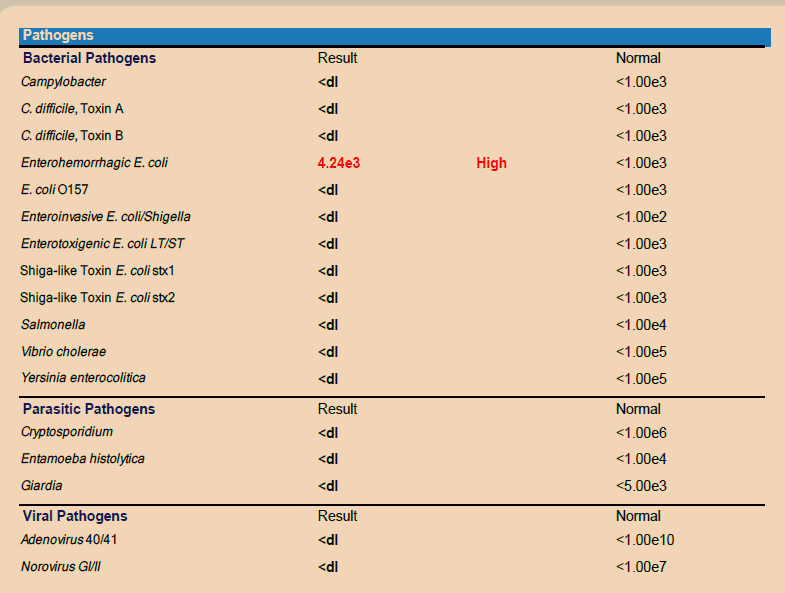
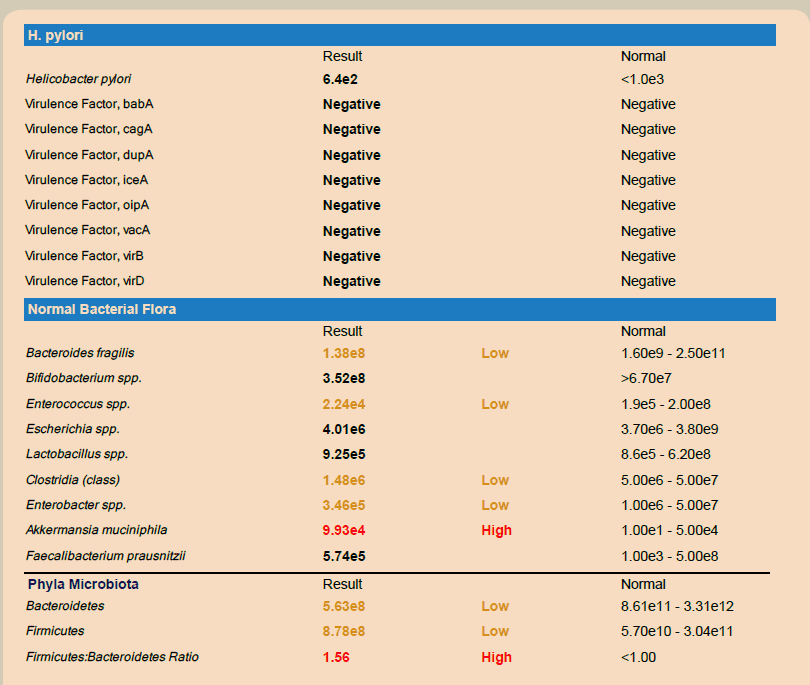
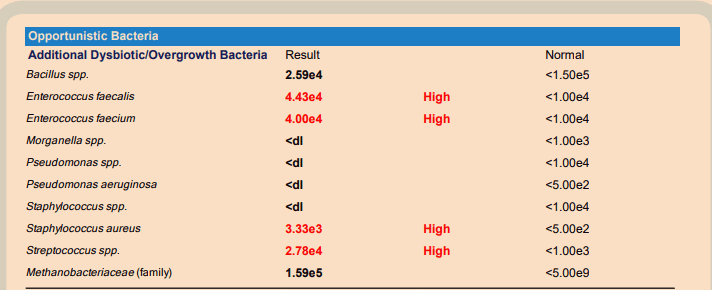
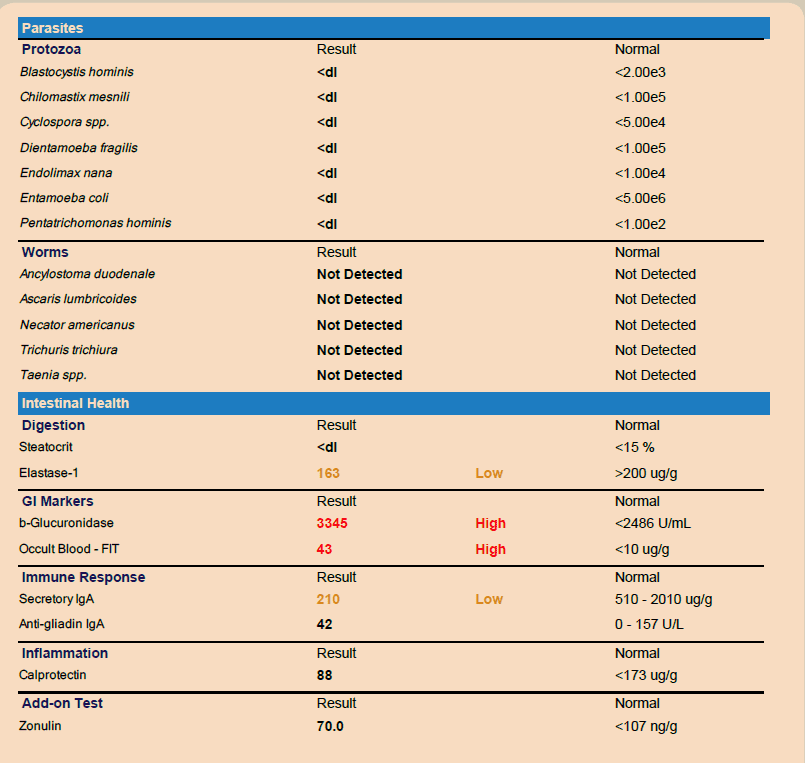
At the start of all of this I had a stool culture test done after having consistent tenesmus and trapped wind/air feeling which lasted all day for weeks. 3-6 bowel movements per day with what felt like paradoxical bowel movements that were hard to get out but were somewhat soft. Went on stool softeners, got diagnosed with IBS and tried some IBS medications (peppermint capsules, simeticone, deflatine) stool testing showed S.T.E.C. antibodies (ecoli antibodies) but I didn't have the typical food poisoning symptoms. Just bad trapped gas and discomfort. Taking activated charcoal gave me bad burning pain around the belly button region - like a square surrounding it.
I've had a small bowel MRI done which showed a normal scan result and when I asked my gastroenterologist he said yes it would also show any stomach or large intestinal problems. He seemed more concerned about malignancy than anything else even though my initial concern was possibly having gelatin stuck somewhere in my system or some kind of other food object.
I have dissolved a gelatin gummy in room temperature water so it doesn't make much sense for there to be gelatin stuck say in my stomach when the human body is typically 36.8C +-1.5C depending on a number of factors (so hot enough to dissolve gelatin gummies)
Had a fairly comprehensive blood panel done and the only things that stood out were high LDL & some thyroid antibody stuff tied to autoimmunity (which ofc my doctors said not to worry about) but I believe the LDL was more tied to a lack of sunlight at the time and my copper and Retinol intake could've been better. Testing it again soon. Thyroid seemed normal, can post if someone wants but will need to find the paperwork.
Two chest x-rays taken, both clear (apparently)
48H ECG machine, normal results. Multiple regular ECGs. Had lungs checked by GP with stethoscope.
I've thought long and hard about what the problem could be and I came up with the following list
GERD
LPR (silent reflux)
Low stomach acid
H.Pylori/Gastritis
SIBO
Hiatus Hernia
Ulcers
Achalasia
R-CPD (retrograde cricopharyngeus dysfunction)
Unknown food intolerance to something really unlikely (like white rice for example)
Unknown issue not on my radar
or a combination which wouldn't be unusual.
Diet before/as this all started happening was as follows
Liver/mince twice a week (about 200g liver a week split to 100g each serving)
Venison multiple times a week or steak
White fish such as Halibut or cod 1-2x a week
Bone broth, Gelatin gummies w/apple juice, Collagen
White rice, Potatoes
Raw goats milk, raw goats kefir (same milk)
Apples, Blueberries, Kiwis (with the gelatin usually),
Raw honey
Dark chocolate, breadsticks (no pufa in them)
Butter, Ghee, Tallow, Olive oil to cook or add to meals (never cooked with the olive oil)
I've gone very restrictive recently after having many debilitating days where I'm in a constant panic state (due to the chest fullness/pressure and breathing) so my diet atm is
Steak
Halibut/Cod/Salmon
Butter, Olive oil, Coconut oil
Apples here and there (have cut them out weeks at a time recently)
Blueberries (have also cut them out before)
Feta cheese
Buffalo Milk Mozzarella
Raw goat milk, experimented with pasteurised and seemingly didn't make any difference. Also cut this out for weeks at a time and I don't seem to react to it aside from a small amount of mucus if I drink too much in one go after having not had it for a while.
Beets which I have recently cut out
Soaked oats which I have recently cut out
White rice which I have recently cut out as well
Goat milk yogurt (pasteurised) which I have recently decided to cut out as well.
As you can see I'm on a slippery slope here where my calories are now starting to fall too low/below my intake goals of about 2700 (1700-2200 atm)
Supplements I take are:
Magnesium (500mg elemental)
Whole food vitamin C 100-300mg
Glycine 5-20g
Thiamine HCL/Benfotiamine at 100mg
Recently started taking PepZinGI (Zinc L-Carnosine) incase it's gastritis i'm suffering from
L-Theanine
Supplements I have but am not currently taking (and will likely add)
Vitamin E
L-Taurine
Pine Pollen Tincture
Digestive enzymes + HCL
Medications I'm on:
Infrequent Propranolol 10-20mg
Experimenting with cyproheptadine at at 1mg dose at night
I have experimented with Betaine HCL from bioptimizers and it seemed to give me minor reflux (acid comes up with the belches) with what seemed like very mild vertigo when I upped the dose from 1 capsule to two. I'm also hesitant to take it or digestive enzymes incase I am suffering from gastritis and unknowingly making it worse.
Symptoms at the start of my problem were:
Woken up in the middle of the night followed by full body shakes and arrythmia/palpitation
Arrhythmias and Palpitations
Trapped gas/air in GI system
Loose stools (bristol stool chart 4.5-6)
Excessive belching leading to trapped air sensation/air hunger/shortness of breath
Dissociative feeling
Now I mostly suffer from
Infrequent Arrythmia and Palpitations
Trapped gas/air in GI system but less painful and less frequent, usually happens stomach and above now
Loose stools when my diet has fibre in it, currently experimenting with removal of carbs and it seems like my bowel movements are type 3-4.5
Belching even on empty stomach with wakeups in the night with mild air hunger (hasn't consistently happened, just sometimes)
Trapped air sensation/air hunger/shortness of breath
Sensation of food in my middle chest (esophagus)
Late bed time due to discomfort & not wanting to lie down. Inclined my bed to help somewhat.
Sometimes the urge to swallow before i've properly chewed my food so I end up swallowing say twice or even 3 times in one fork/mouthful of food
Very frustrated as I've been battling with this for months and have no idea what it is yet. The discomfort is really bad to the point i've gone to the ER several times and I can be in discomfort for days at a time with very little relief sometimes (the air hunger issue). Since I don't know what the issue is I don't know what I can do about it.
Wondering if anyone has dealt with anything similar to this and if so, what is was and how you treated it. Or just input in general, I'm running out of ideas & hope.
It seemingly spontaneously started happening when I was going pretty heavy on High vitamin K doses and also on high histamine foods (bone broth, gelatin, kefir, dark chocolate) but I have since stopped eating gelatin, bone broth, dark chocolate and kefir I was having up until very recently but have cut that out too since it's gassy and makes me burp which makes the likelihood of it getting trapped more likely. I remember switching from blueberry juice to apple juice for my gelatin gummies and that's when I really started to notice it happening. Since then the belching has decreased in frequency and strength (the belches are smaller) but the issue with this is it seems like they can sometimes get stuck in my esophagus/chest
The worst part about it is the air sometimes gets stuck in my esophagus/chest and it feels like I cannot breathe properly. This activates anxiety and I start manually breathing with the constant air hunger feeling. The belches can sometimes be very very small, like 20% the size of a regular belch.
At the start of all of this I had a stool culture test done after having consistent tenesmus and trapped wind/air feeling which lasted all day for weeks. 3-6 bowel movements per day with what felt like paradoxical bowel movements that were hard to get out but were somewhat soft. Went on stool softeners, got diagnosed with IBS and tried some IBS medications (peppermint capsules, simeticone, deflatine) stool testing showed S.T.E.C. antibodies (ecoli antibodies) but I didn't have the typical food poisoning symptoms. Just bad trapped gas and discomfort. Taking activated charcoal gave me bad burning pain around the belly button region - like a square surrounding it.
I've had a small bowel MRI done which showed a normal scan result and when I asked my gastroenterologist he said yes it would also show any stomach or large intestinal problems. He seemed more concerned about malignancy than anything else even though my initial concern was possibly having gelatin stuck somewhere in my system or some kind of other food object.
I have dissolved a gelatin gummy in room temperature water so it doesn't make much sense for there to be gelatin stuck say in my stomach when the human body is typically 36.8C +-1.5C depending on a number of factors (so hot enough to dissolve gelatin gummies)
Had a fairly comprehensive blood panel done and the only things that stood out were high LDL & some thyroid antibody stuff tied to autoimmunity (which ofc my doctors said not to worry about) but I believe the LDL was more tied to a lack of sunlight at the time and my copper and Retinol intake could've been better. Testing it again soon. Thyroid seemed normal, can post if someone wants but will need to find the paperwork.
Two chest x-rays taken, both clear (apparently)
48H ECG machine, normal results. Multiple regular ECGs. Had lungs checked by GP with stethoscope.
I've thought long and hard about what the problem could be and I came up with the following list
GERD
LPR (silent reflux)
Low stomach acid
H.Pylori/Gastritis
SIBO
Hiatus Hernia
Ulcers
Achalasia
R-CPD (retrograde cricopharyngeus dysfunction)
Unknown food intolerance to something really unlikely (like white rice for example)
Unknown issue not on my radar
or a combination which wouldn't be unusual.
Diet before/as this all started happening was as follows
Liver/mince twice a week (about 200g liver a week split to 100g each serving)
Venison multiple times a week or steak
White fish such as Halibut or cod 1-2x a week
Bone broth, Gelatin gummies w/apple juice, Collagen
White rice, Potatoes
Raw goats milk, raw goats kefir (same milk)
Apples, Blueberries, Kiwis (with the gelatin usually),
Raw honey
Dark chocolate, breadsticks (no pufa in them)
Butter, Ghee, Tallow, Olive oil to cook or add to meals (never cooked with the olive oil)
I've gone very restrictive recently after having many debilitating days where I'm in a constant panic state (due to the chest fullness/pressure and breathing) so my diet atm is
Steak
Halibut/Cod/Salmon
Butter, Olive oil, Coconut oil
Apples here and there (have cut them out weeks at a time recently)
Blueberries (have also cut them out before)
Feta cheese
Buffalo Milk Mozzarella
Raw goat milk, experimented with pasteurised and seemingly didn't make any difference. Also cut this out for weeks at a time and I don't seem to react to it aside from a small amount of mucus if I drink too much in one go after having not had it for a while.
Beets which I have recently cut out
Soaked oats which I have recently cut out
White rice which I have recently cut out as well
Goat milk yogurt (pasteurised) which I have recently decided to cut out as well.
As you can see I'm on a slippery slope here where my calories are now starting to fall too low/below my intake goals of about 2700 (1700-2200 atm)
Supplements I take are:
Magnesium (500mg elemental)
Whole food vitamin C 100-300mg
Glycine 5-20g
Thiamine HCL/Benfotiamine at 100mg
Recently started taking PepZinGI (Zinc L-Carnosine) incase it's gastritis i'm suffering from
L-Theanine
Supplements I have but am not currently taking (and will likely add)
Vitamin E
L-Taurine
Pine Pollen Tincture
Digestive enzymes + HCL
Medications I'm on:
Infrequent Propranolol 10-20mg
Experimenting with cyproheptadine at at 1mg dose at night
I have experimented with Betaine HCL from bioptimizers and it seemed to give me minor reflux (acid comes up with the belches) with what seemed like very mild vertigo when I upped the dose from 1 capsule to two. I'm also hesitant to take it or digestive enzymes incase I am suffering from gastritis and unknowingly making it worse.
Symptoms at the start of my problem were:
Woken up in the middle of the night followed by full body shakes and arrythmia/palpitation
Arrhythmias and Palpitations
Trapped gas/air in GI system
Loose stools (bristol stool chart 4.5-6)
Excessive belching leading to trapped air sensation/air hunger/shortness of breath
Dissociative feeling
Now I mostly suffer from
Infrequent Arrythmia and Palpitations
Trapped gas/air in GI system but less painful and less frequent, usually happens stomach and above now
Loose stools when my diet has fibre in it, currently experimenting with removal of carbs and it seems like my bowel movements are type 3-4.5
Belching even on empty stomach with wakeups in the night with mild air hunger (hasn't consistently happened, just sometimes)
Trapped air sensation/air hunger/shortness of breath
Sensation of food in my middle chest (esophagus)
Late bed time due to discomfort & not wanting to lie down. Inclined my bed to help somewhat.
Sometimes the urge to swallow before i've properly chewed my food so I end up swallowing say twice or even 3 times in one fork/mouthful of food
Very frustrated as I've been battling with this for months and have no idea what it is yet. The discomfort is really bad to the point i've gone to the ER several times and I can be in discomfort for days at a time with very little relief sometimes (the air hunger issue). Since I don't know what the issue is I don't know what I can do about it.
Wondering if anyone has dealt with anything similar to this and if so, what is was and how you treated it. Or just input in general, I'm running out of ideas & hope.
Last edited: