Mito
Member
- Joined
- Dec 10, 2016
- Messages
- 2,554
Follow along with the video below to see how to install our site as a web app on your home screen.
Note: This feature may not be available in some browsers.
Click Here if you want to upgrade your account
If you were able to post but cannot do so now, send an email to admin at raypeatforum dot com and include your username and we will fix that right up for you.
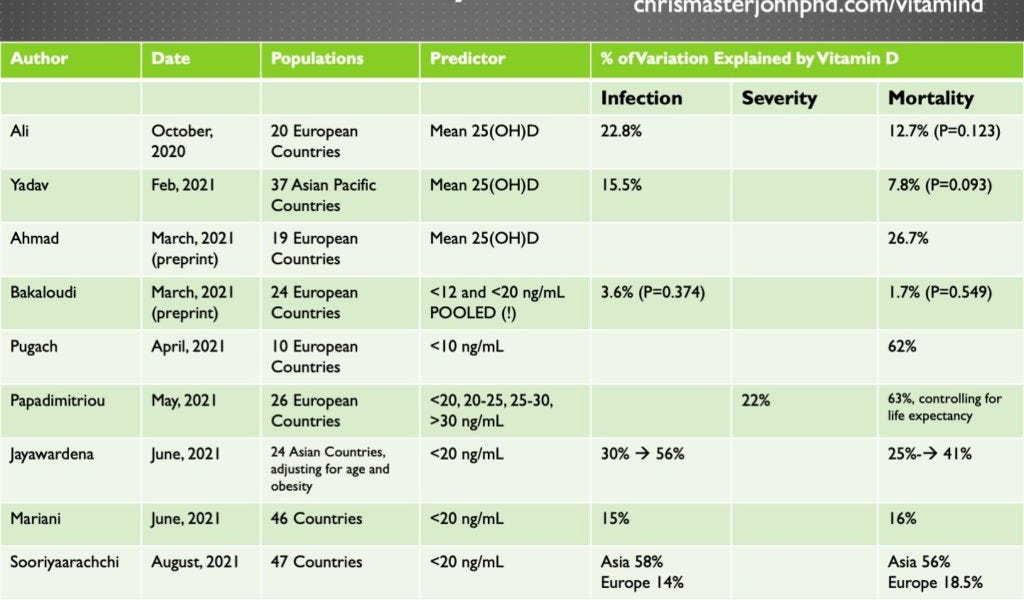
This is a helpful summary. Thank youOverall Conclusions
Synthesizing all of the data, we can conclude as follows:
- While the threat of COVID-19 persists, actively maintaining 25(OH)D in the 30-60 ng/mL range is likely to protect against getting infected, with the best protection offered in the 50-60 ng/mL range.
- Whether a supplement is needed to maintain this and how much depends on one's environment, lifestyle, diet, and other factors, so it is best to measure the blood level. Many people living in temperate regions would require 5,000 IU per day during the coldest half of the year.
- Maintaining D in this range will also prevent a 5-or-more-day delay in the ability to quickly raise 25(OH)D with vitamin D supplements upon getting sick.
- If the Entrenas-Castillo protocol is adjusted for the relative bioavailability of 25(OH)D and vitamin D and converted into the equivalent of oral vitamin D3 supplements, it translates to 106,400 IU on day 1, 53,200 IU on days 3 and 7, and 53,200 IU per week thereafter until symptoms resolve. If this is in turn translated into daily dosing, it would be the equivalent of 30,400 IU per day for the first week, followed by a maintenance dose of 7,600 IU per day until symptoms resolve. This could be simplified to a loading dose of 200,000 IU once, followed by a 10,000 IU per day maintenance dose until symptoms resolve.
- This protocol should be started at the first sign of any possible symptom and should not be delayed until COVID-19 is confirmed. This is needed to raise biological vitamin D activity at the beginning of the infection, rather than waiting until it is a) too late and b) too difficult to raise 25(OH)D in an environment of excessive inflammation.
- For someone who is maintaining 25(OH)D in the 50-60 ng/mL range, the loading dose might be unnecessary. However, for anyone with 25(OH)D lower than this, the loading dose is critical. For someone who is likely deficient at the time of infection and waits until diagnosed or hospitalized before starting vitamin D, it is imperative for a physician to prescribe calcifediol (that is, oral 25(OH)D) at a dose of 0.532 miligrams on day 1, followed by 0.266 milligrams on days 3 and 7, and weekly thereafter until symptoms resolve.
- Although concrete evidence for this is lacking, my personal opinion is that each 10,000 IU of vitamin D (the loading dose can be excepted from this) should be matched with 5-10,000 IU of vitamin A (as retinol), 200 micrograms of vitamin K2 (preferably as a mix of MK-4 and MK-7), and 20 IU of alpha-tocopherol in a background of naturally occurring mixed tocopherols and tocotrienols. The diet should be analyzed (for example, as described here) to make sure that no nutrients are deficient and zinc dosing as described here should be considered.
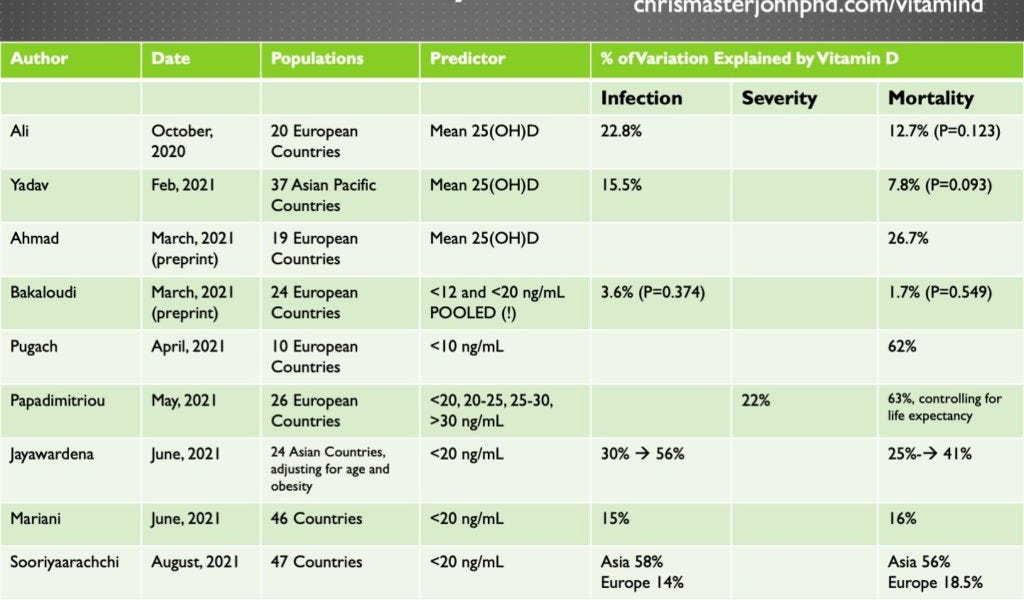
Vitamin D and COVID-19: The Current State of the Evidence
Note: You can watch my presentation based on this research from the 2021 Ancestral Health Symposium here, watch a much longer video that covers missing slides and answers questions about the talk here, download a PDF of my slides here, and see a short list of minor corrections to the presentation inchrismasterjohnphd.com

Is this only an issue for those who notice bad effects from MCT? I've been using an MCT-based D3 supplement and haven't noticed any adverse reactions. I'm always skeptical that olive oil is really olive oil, though the capsules are so small that it probably doesn't matter.Ray talked about this in a recent interview with Danny and Georgi, olive oil probably solves much of the allergenic reaction with MCT.

 chrismasterjohnphd.com
chrismasterjohnphd.com

 chrismasterjohnphd.com
chrismasterjohnphd.com
Not sure what he had. But he survived, twiceNot sure I'd follow his protocol, he got COVID twice, so far.
But, someone his age, unless with serious underlying conditions, shouldn't have to follow any "protocol" to survive. Of all the people his age I personally know that got it, not a single one had to take anything more than aspirin, for what was basically a moderate cold.Not sure what he had. But he survived, twice
From what I recall he had some sort of environmental toxin/mold issue, I suspect that’s left his immune system compromised. Being exposed to mold is no small thing.But, someone his age, unless with serious underlying conditions, shouldn't have to follow any "protocol" to survive. Of all the people his age I personally know that got it, not a single one had to take anything more than aspirin, for what was basically a moderate cold.
This is so true. Appreciate your example of the Vit D.Rays always ahead of the game.