Obi-wan
Member
- Joined
- Mar 16, 2017
- Messages
- 1,120
Vitamin D
From Wikipedia, the free encyclopedia
Jump to navigation Jump to search
For other uses, see Vitamin D (disambiguation).
Vitamin D
Drug class
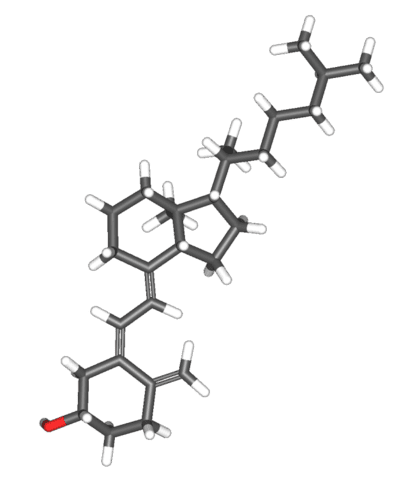
Cholecalciferol (D3)
Class identifiers
Use Rickets, osteoporosis, vitamin D deficiency
ATC code A11CC
Biological target vitamin D receptor
Clinical data
Drugs.com MedFacts Natural Products
External links
MeSH D014807
In Wikidata
Vitamin D is a group of fat-soluble secosteroids responsible for increasing intestinal absorption of calcium, magnesium, and phosphate, and multiple other biological effects.[1] In humans, the most important compounds in this group are vitamin D3 (also known as cholecalciferol) and vitamin D2 (ergocalciferol).[2] Cholecalciferol and ergocalciferol can be ingested from the diet and from supplements.[2][3][4] Only a few foods contain vitamin D. The major natural source of the vitamin is synthesis of cholecalciferol in the skin from cholesterol through a chemical reaction that is dependent on sun exposure (specifically UVB radiation). Dietary recommendations typically assume that all of a person's vitamin D is taken by mouth, as sun exposure in the population is variable and recommendations about the amount of sun exposure that is safe are uncertain in view of the skin cancer risk.[5]
Vitamin D from the diet or skin synthesis is biologically inactive; enzymatic conversion (hydroxylation) in the liver and kidney is required for activation. As vitamin D can be synthesized in adequate amounts by most mammals exposed to sufficient sunlight, it is not an essential dietary factor, and so not technically a vitamin.[4] Instead it could be considered as a hormone, with activation of the vitamin D pro-hormone resulting in the active form, calcitriol, which then produces effects via a nuclear receptor in multiple different locations.[4] Cholecalciferol is converted in the liver to calcifediol (25-hydroxycholecalciferol); ergocalciferol is converted to 25-hydroxyergocalciferol. These two vitamin D metabolites (called 25-hydroxyvitamin D or 25(OH)D) are measured in serum to determine a person's vitamin D status.[6][7] Calcifediol is further hydroxylated by the kidneys to form calcitriol (also known as 1,25-dihydroxycholecalciferol), the biologically active form of vitamin D.[8] Calcitriol circulates as a hormone in the blood, having a major role regulating the concentration of calcium and phosphate, and promoting the healthy growth and remodeling of bone. Calcitriol also has other effects, including some on cell growth, neuromuscular and immune functions, and reduction of inflammation.[5]
Vitamin D has a significant role in calcium homeostasis and metabolism. Its discovery was due to effort to find the dietary substance lacking in children with rickets (the childhood form of osteomalacia).[9] Vitamin D supplements are given to treat or to prevent osteomalacia and rickets, but the evidence for other health effects of vitamin D supplementation in the general population is inconsistent.[10][11] The effect of vitamin D supplementation on mortality is not clear, with one meta-analysis finding a small decrease in mortality in elderly people,[12] and another concluding no clear justification exists for recommending supplementation for preventing many diseases, and that further research of similar design is unneeded in these areas.[13]
Excess[edit]
Further information: hypervitaminosis D
Vitamin D toxicity is rare.[24] It is caused by supplementing with high doses of vitamin D rather than sunlight. The threshold for vitamin D toxicity has not been established; however, according to some research, the tolerable upper intake level (UL) is 4,000 IU/day for ages 9–71[139] (100 µg/day), while other research concludes that, in healthy adults, sustained intake of more than 1250 μg/day (50,000 IU) can produce overt toxicity after several months and can increase serum 25-hydroxyvitamin D levels to 150 ng/ml and greater.[24][140] Those with certain medical conditions, such as primary hyperparathyroidism,[141] are far more sensitive to vitamin D and develop hypercalcemia in response to any increase in vitamin D nutrition, while maternal hypercalcemia during pregnancy may increase fetal sensitivity to effects of vitamin D and lead to a syndrome of mental retardation and facial deformities.[141][142]
A review published in 2015 noted that adverse effects have been reported only at 25(OH)D serum concentrations above 200 nmol/L.[136]
Published cases of toxicity involving hypercalcemia in which the vitamin D dose and the 25-hydroxy-vitamin D levels are known all involve an intake of ≥40,000 IU (1,000 μg) per day.[141]
Pregnant or breastfeeding women should consult a doctor before taking a vitamin D supplement. The FDA advised manufacturers of liquid vitamin D supplements that droppers accompanying these products should be clearly and accurately marked for 400 international units (1 IU is the biological equivalent of 25 ng cholecalciferol/ergocalciferol). In addition, for products intended for infants, the FDA recommends the dropper hold no more than 400 IU.[143] For infants (birth to 12 months), the tolerable upper limit (maximum amount that can be tolerated without harm) is set at 25 μg/day (1,000 IU). One thousand micrograms per day in infants has produced toxicity within one month.[140] After being commissioned by the Canadian and American governments, the Institute of Medicine (IOM) as of 30 November 2010, has increased the tolerable upper limit (UL) to 2,500 IU per day for ages 1–3 years, 3,000 IU per day for ages 4–8 years and 4,000 IU per day for ages 9–71+ years (including pregnant or lactating women).[139]
Calcitriol itself is auto-regulated in a negative feedback cycle, and is also affected by parathyroid hormone, fibroblast growth factor 23, cytokines, calcium, and phosphate.[144]
Effect of excess[edit]
Vitamin D overdose causes hypercalcemia, which is a strong indication of vitamin D toxicity – this can be noted with an increase in urination and thirst. If hypercalcemia is not treated, it results in excess deposits of calcium in soft tissues and organs such as the kidneys, liver, and heart, resulting in pain and organ damage.[24][27][44]
The main symptoms of vitamin D overdose which are those of hypercalcemia including anorexia, nausea, and vomiting. These may be followed by polyuria, polydipsia, weakness, insomnia, nervousness, pruritus and ultimately renal failure. Furthermore, proteinuria, urinary casts, azotemia, and metastatic calcification (especially in the kidneys) may develop.[140] Other symptoms of vitamin D toxicity include mental retardation in young children, abnormal bone growth and formation, diarrhea, irritability, weight loss, and severe depression.[24][44]
Vitamin D toxicity is treated by discontinuing vitamin D supplementation and restricting calcium intake. Kidney damage may be irreversible. Exposure to sunlight for extended periods of time does not normally cause vitamin D toxicity. The concentrations of vitamin D precursors produced in the skin reach an equilibrium, and any further vitamin D produced is degraded.[141]
Sunscreen absorbs or reflects ultraviolet light and prevents much of it from reaching the skin.[156] Sunscreen with a sun protection factor (SPF) of 8 based on the UVB spectrum decreases vitamin D synthetic capacity by 95%, and SPF 15 decreases it by 98%.[157]
I would be carful with both Vit D supplementation and Calcium supplementation... My mother got hypercalcemia (calcium dumped into her blood) and had one of her parathyroid's removed. You have 4 on your thyroid.
From Wikipedia, the free encyclopedia
Jump to navigation Jump to search
For other uses, see Vitamin D (disambiguation).
Vitamin D
Drug class
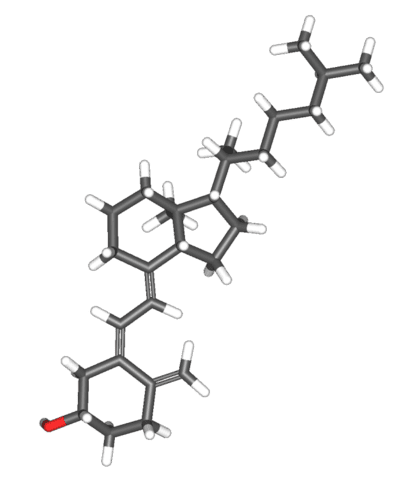
Cholecalciferol (D3)
Class identifiers
Use Rickets, osteoporosis, vitamin D deficiency
ATC code A11CC
Biological target vitamin D receptor
Clinical data
Drugs.com MedFacts Natural Products
External links
MeSH D014807
In Wikidata
Vitamin D is a group of fat-soluble secosteroids responsible for increasing intestinal absorption of calcium, magnesium, and phosphate, and multiple other biological effects.[1] In humans, the most important compounds in this group are vitamin D3 (also known as cholecalciferol) and vitamin D2 (ergocalciferol).[2] Cholecalciferol and ergocalciferol can be ingested from the diet and from supplements.[2][3][4] Only a few foods contain vitamin D. The major natural source of the vitamin is synthesis of cholecalciferol in the skin from cholesterol through a chemical reaction that is dependent on sun exposure (specifically UVB radiation). Dietary recommendations typically assume that all of a person's vitamin D is taken by mouth, as sun exposure in the population is variable and recommendations about the amount of sun exposure that is safe are uncertain in view of the skin cancer risk.[5]
Vitamin D from the diet or skin synthesis is biologically inactive; enzymatic conversion (hydroxylation) in the liver and kidney is required for activation. As vitamin D can be synthesized in adequate amounts by most mammals exposed to sufficient sunlight, it is not an essential dietary factor, and so not technically a vitamin.[4] Instead it could be considered as a hormone, with activation of the vitamin D pro-hormone resulting in the active form, calcitriol, which then produces effects via a nuclear receptor in multiple different locations.[4] Cholecalciferol is converted in the liver to calcifediol (25-hydroxycholecalciferol); ergocalciferol is converted to 25-hydroxyergocalciferol. These two vitamin D metabolites (called 25-hydroxyvitamin D or 25(OH)D) are measured in serum to determine a person's vitamin D status.[6][7] Calcifediol is further hydroxylated by the kidneys to form calcitriol (also known as 1,25-dihydroxycholecalciferol), the biologically active form of vitamin D.[8] Calcitriol circulates as a hormone in the blood, having a major role regulating the concentration of calcium and phosphate, and promoting the healthy growth and remodeling of bone. Calcitriol also has other effects, including some on cell growth, neuromuscular and immune functions, and reduction of inflammation.[5]
Vitamin D has a significant role in calcium homeostasis and metabolism. Its discovery was due to effort to find the dietary substance lacking in children with rickets (the childhood form of osteomalacia).[9] Vitamin D supplements are given to treat or to prevent osteomalacia and rickets, but the evidence for other health effects of vitamin D supplementation in the general population is inconsistent.[10][11] The effect of vitamin D supplementation on mortality is not clear, with one meta-analysis finding a small decrease in mortality in elderly people,[12] and another concluding no clear justification exists for recommending supplementation for preventing many diseases, and that further research of similar design is unneeded in these areas.[13]
Excess[edit]
Further information: hypervitaminosis D
Vitamin D toxicity is rare.[24] It is caused by supplementing with high doses of vitamin D rather than sunlight. The threshold for vitamin D toxicity has not been established; however, according to some research, the tolerable upper intake level (UL) is 4,000 IU/day for ages 9–71[139] (100 µg/day), while other research concludes that, in healthy adults, sustained intake of more than 1250 μg/day (50,000 IU) can produce overt toxicity after several months and can increase serum 25-hydroxyvitamin D levels to 150 ng/ml and greater.[24][140] Those with certain medical conditions, such as primary hyperparathyroidism,[141] are far more sensitive to vitamin D and develop hypercalcemia in response to any increase in vitamin D nutrition, while maternal hypercalcemia during pregnancy may increase fetal sensitivity to effects of vitamin D and lead to a syndrome of mental retardation and facial deformities.[141][142]
A review published in 2015 noted that adverse effects have been reported only at 25(OH)D serum concentrations above 200 nmol/L.[136]
Published cases of toxicity involving hypercalcemia in which the vitamin D dose and the 25-hydroxy-vitamin D levels are known all involve an intake of ≥40,000 IU (1,000 μg) per day.[141]
Pregnant or breastfeeding women should consult a doctor before taking a vitamin D supplement. The FDA advised manufacturers of liquid vitamin D supplements that droppers accompanying these products should be clearly and accurately marked for 400 international units (1 IU is the biological equivalent of 25 ng cholecalciferol/ergocalciferol). In addition, for products intended for infants, the FDA recommends the dropper hold no more than 400 IU.[143] For infants (birth to 12 months), the tolerable upper limit (maximum amount that can be tolerated without harm) is set at 25 μg/day (1,000 IU). One thousand micrograms per day in infants has produced toxicity within one month.[140] After being commissioned by the Canadian and American governments, the Institute of Medicine (IOM) as of 30 November 2010, has increased the tolerable upper limit (UL) to 2,500 IU per day for ages 1–3 years, 3,000 IU per day for ages 4–8 years and 4,000 IU per day for ages 9–71+ years (including pregnant or lactating women).[139]
Calcitriol itself is auto-regulated in a negative feedback cycle, and is also affected by parathyroid hormone, fibroblast growth factor 23, cytokines, calcium, and phosphate.[144]
Effect of excess[edit]
Vitamin D overdose causes hypercalcemia, which is a strong indication of vitamin D toxicity – this can be noted with an increase in urination and thirst. If hypercalcemia is not treated, it results in excess deposits of calcium in soft tissues and organs such as the kidneys, liver, and heart, resulting in pain and organ damage.[24][27][44]
The main symptoms of vitamin D overdose which are those of hypercalcemia including anorexia, nausea, and vomiting. These may be followed by polyuria, polydipsia, weakness, insomnia, nervousness, pruritus and ultimately renal failure. Furthermore, proteinuria, urinary casts, azotemia, and metastatic calcification (especially in the kidneys) may develop.[140] Other symptoms of vitamin D toxicity include mental retardation in young children, abnormal bone growth and formation, diarrhea, irritability, weight loss, and severe depression.[24][44]
Vitamin D toxicity is treated by discontinuing vitamin D supplementation and restricting calcium intake. Kidney damage may be irreversible. Exposure to sunlight for extended periods of time does not normally cause vitamin D toxicity. The concentrations of vitamin D precursors produced in the skin reach an equilibrium, and any further vitamin D produced is degraded.[141]
Sunscreen absorbs or reflects ultraviolet light and prevents much of it from reaching the skin.[156] Sunscreen with a sun protection factor (SPF) of 8 based on the UVB spectrum decreases vitamin D synthetic capacity by 95%, and SPF 15 decreases it by 98%.[157]
I would be carful with both Vit D supplementation and Calcium supplementation... My mother got hypercalcemia (calcium dumped into her blood) and had one of her parathyroid's removed. You have 4 on your thyroid.
