Hi guys,
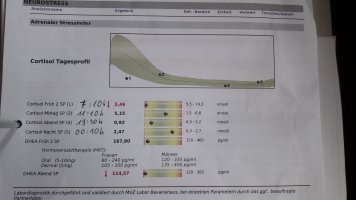
I'm new to the forum and also kind of new to Ray Peat ideas, I started digging into it in summer 2022. My understanding of physiology/bio chemistry is limited, in regards to Peats ideas I think i get the basic paradigm and some of the basic ideas and recommendations. However, I have a hard time bringing the pieces together to help myself. I have a history of burnout (first breakdown in 2016 being 27 years old), I'm now 33, male, and have had multiple crashes/relapses in the past couple years where I have been bedridden for weeks to months until I very slowly got better again. So basically something like adrenal fatigue (I know of the shortcomings of the term) or chronic fatigue syndrome, but without the virus/infection element. Unfortunately, going through all these relapses in the recent years, my condition overall has worsened. Stress of any kind is the biggest killer for me, it leads to PEM (post exertional malaise) when I overdo it. Right now I'm near the next relapse, as here in Germany where I live the days are getting shorter and darker. Sunlight/bright light and summer time have a positive effect on my condition, so fall/autumn and winter always make me worse. So basically, the only tools I had in the past years were stress mitigation and sunlight exposure, esp. in the morning. But they both have their limits. I tried thyroid T4/T3 combination and NDT (metavive), up to 70mcg T4/12.5mcg T3 or 1.25 grains, respectively, they did only a little improvement, but they didn't give me that underlying stamina or stability in energy levels. For example, I mostly avoid lifting heavy stuff or walking the stairs too often, as they deplete me of my energy the most. Thyroid medication had only a small effect on that. I always suspected that it must be low cortisol and in fact, I had multiple saliva profiles made in the past years and 4 out 5 showed very low levels, someteimes below reference range. Problem always was I didn't know what to do with it. I went to 2 different pracitioners andone only recommended taking amino acids, the other saw no big problem with my lowish or even the clearly low levels. Now I have too little power left to start a new appointment at someones office.
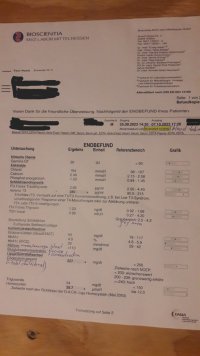
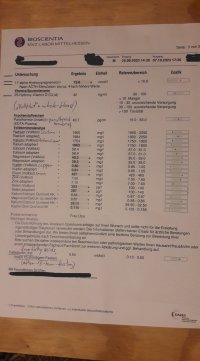
I attached my latest lab works. Please feel free to comment and if possible, please add some rationale or explenation if you want to share some interpretations or advice, so that I have a chance to make better decisions. I started taking advice from Paul Robinson (kind of prominent for his circadian T3 method CT3M), his recommendations are also based on the attached lab work and my story.
Here are some additional information that might be important for interpreting the lab results and my overall condition right now:
- When I had the first big crash in 2020, my body ramped up my appetite and I had to eat like crazy: 5 big meals daily, so every 3 hours. And I mean BIG, ca. 120 grams carbohydrates plus 100 grams fat, so in total 600g carbs, 500 fat EVERY DAY for 8 weeks, then it went down to 4 times a day this big meal. My blood cortisol was at 8.8 at that time, so very low, at the same time i suspect that my thyroid hormones were still working, that's why the big demand? Because cortisol couldn't keep up the blood sugar anymore? And the big amount of fat maybe had some signaling function? - When I got better over time, the frequency and amount of food went down again to my normal levels (3 main meals plus maybe one snack in the afternoon).
- The same thing happened every new crash since 2020: the frequency and amount of food that my body thought was necesarry went up on the day I crashed (you can believe me, the signals my body sent were unambiguous. If I was eating only slightly less than my body said I should, I risked another energy crisis which could easily lead to further deterioration). Of course I always gained weight, from my average 63kg when I was a normal healthy person to around 80kg or above. And note , I am naturally a lean, slim guy who never had been able to put on weight, even if I wanted to.
- In 2022 the crash was a bit different; meal frequency went up again, but 'only' to 4 times a day. Again, mainly carbs plus a lot of fat. Protein didn't work for me, my body told me that. When I started taking venlafaxine out of desperation, as it was the only medication I took during my first clinic stay in 2020, I only had to eat three times per day again. That was kind of a relief because I was so exhausted and worn out that it was a battle every time to get up and get something to eat. My theory is that the increase of serotonin by taking venlafaxine had something to do with it. Interestingly, the meal frequency went down to only 2 times a day, normal meal size. So after this crash and partly regeneration, I was forced by my body to eat less than at any time in my life before.
- Now we're nearing my current situation: The latest crash in spring 2023 at first caused a short increase in meal quantity again (this time not in frequency though), and another reduction when I improved again. So this is where I'm at now: Only one meal per day, late in the evening, of the size of 1.5 to 2 normal meals. The least amount I was ever eating per day. I am feeling full in my belly all day long until 10 PM at night. At the same time, my stamina, energy and resilience against stress is further diminished compared to the periods in 2022 or 2021 after recovery of the respective crash.
My overall hypothesis: I am now in fat burning mode (elevated free fatty acids on my lab) all day long. That means oxidative metabolism of sugar is reduced significantly (see my low insulin and low hba1c) and I must rely on cortisol for blood sugar regulation and/or releasing of free fatty acids for energy production. But unfortunately, my cortisol is still low after all these crashes (blood AND saliva results), therefore even the inefficent metabolic mode the body chooses to go into because of stress can't work properly, that's why I am feeling so bad (low stamina, resilience etc.) even on better days.
What are your thoughts? I am grateful for any advice, thanks!
I'm new to the forum and also kind of new to Ray Peat ideas, I started digging into it in summer 2022. My understanding of physiology/bio chemistry is limited, in regards to Peats ideas I think i get the basic paradigm and some of the basic ideas and recommendations. However, I have a hard time bringing the pieces together to help myself. I have a history of burnout (first breakdown in 2016 being 27 years old), I'm now 33, male, and have had multiple crashes/relapses in the past couple years where I have been bedridden for weeks to months until I very slowly got better again. So basically something like adrenal fatigue (I know of the shortcomings of the term) or chronic fatigue syndrome, but without the virus/infection element. Unfortunately, going through all these relapses in the recent years, my condition overall has worsened. Stress of any kind is the biggest killer for me, it leads to PEM (post exertional malaise) when I overdo it. Right now I'm near the next relapse, as here in Germany where I live the days are getting shorter and darker. Sunlight/bright light and summer time have a positive effect on my condition, so fall/autumn and winter always make me worse. So basically, the only tools I had in the past years were stress mitigation and sunlight exposure, esp. in the morning. But they both have their limits. I tried thyroid T4/T3 combination and NDT (metavive), up to 70mcg T4/12.5mcg T3 or 1.25 grains, respectively, they did only a little improvement, but they didn't give me that underlying stamina or stability in energy levels. For example, I mostly avoid lifting heavy stuff or walking the stairs too often, as they deplete me of my energy the most. Thyroid medication had only a small effect on that. I always suspected that it must be low cortisol and in fact, I had multiple saliva profiles made in the past years and 4 out 5 showed very low levels, someteimes below reference range. Problem always was I didn't know what to do with it. I went to 2 different pracitioners andone only recommended taking amino acids, the other saw no big problem with my lowish or even the clearly low levels. Now I have too little power left to start a new appointment at someones office.
I attached my latest lab works. Please feel free to comment and if possible, please add some rationale or explenation if you want to share some interpretations or advice, so that I have a chance to make better decisions. I started taking advice from Paul Robinson (kind of prominent for his circadian T3 method CT3M), his recommendations are also based on the attached lab work and my story.
Here are some additional information that might be important for interpreting the lab results and my overall condition right now:
- When I had the first big crash in 2020, my body ramped up my appetite and I had to eat like crazy: 5 big meals daily, so every 3 hours. And I mean BIG, ca. 120 grams carbohydrates plus 100 grams fat, so in total 600g carbs, 500 fat EVERY DAY for 8 weeks, then it went down to 4 times a day this big meal. My blood cortisol was at 8.8 at that time, so very low, at the same time i suspect that my thyroid hormones were still working, that's why the big demand? Because cortisol couldn't keep up the blood sugar anymore? And the big amount of fat maybe had some signaling function? - When I got better over time, the frequency and amount of food went down again to my normal levels (3 main meals plus maybe one snack in the afternoon).
- The same thing happened every new crash since 2020: the frequency and amount of food that my body thought was necesarry went up on the day I crashed (you can believe me, the signals my body sent were unambiguous. If I was eating only slightly less than my body said I should, I risked another energy crisis which could easily lead to further deterioration). Of course I always gained weight, from my average 63kg when I was a normal healthy person to around 80kg or above. And note , I am naturally a lean, slim guy who never had been able to put on weight, even if I wanted to.
- In 2022 the crash was a bit different; meal frequency went up again, but 'only' to 4 times a day. Again, mainly carbs plus a lot of fat. Protein didn't work for me, my body told me that. When I started taking venlafaxine out of desperation, as it was the only medication I took during my first clinic stay in 2020, I only had to eat three times per day again. That was kind of a relief because I was so exhausted and worn out that it was a battle every time to get up and get something to eat. My theory is that the increase of serotonin by taking venlafaxine had something to do with it. Interestingly, the meal frequency went down to only 2 times a day, normal meal size. So after this crash and partly regeneration, I was forced by my body to eat less than at any time in my life before.
- Now we're nearing my current situation: The latest crash in spring 2023 at first caused a short increase in meal quantity again (this time not in frequency though), and another reduction when I improved again. So this is where I'm at now: Only one meal per day, late in the evening, of the size of 1.5 to 2 normal meals. The least amount I was ever eating per day. I am feeling full in my belly all day long until 10 PM at night. At the same time, my stamina, energy and resilience against stress is further diminished compared to the periods in 2022 or 2021 after recovery of the respective crash.
My overall hypothesis: I am now in fat burning mode (elevated free fatty acids on my lab) all day long. That means oxidative metabolism of sugar is reduced significantly (see my low insulin and low hba1c) and I must rely on cortisol for blood sugar regulation and/or releasing of free fatty acids for energy production. But unfortunately, my cortisol is still low after all these crashes (blood AND saliva results), therefore even the inefficent metabolic mode the body chooses to go into because of stress can't work properly, that's why I am feeling so bad (low stamina, resilience etc.) even on better days.
What are your thoughts? I am grateful for any advice, thanks!