Navigation
Install the app
How to install the app on iOS
Follow along with the video below to see how to install our site as a web app on your home screen.
Note: This feature may not be available in some browsers.
More options
-
By using this site you agree to the terms, rules, and privacy policy.
-
Charlie's Restoration Giveaway #2 (Entire Home EMF Mitigation & Protection Along With Personal Protection) - Click Here To Enter
-
Dear Carnivore Dieters, A Muscle Meat Only Diet is Extremely Healing Because it is a Low "vitamin A" Diet. This is Why it Works so Well...
Rest the rest of this post by clicking here
-
The Forum is transitioning to a subscription-based membership model - Click Here To Read
Click Here if you want to upgrade your account
If you were able to post but cannot do so now, send an email to admin at raypeatforum dot com and include your username and we will fix that right up for you.
You are using an out of date browser. It may not display this or other websites correctly.
You should upgrade or use an alternative browser.
You should upgrade or use an alternative browser.
Histamine Potentiates SARS-CoV-2 Spike Protein Entry Into Endothelial Cells
- Thread starter Jam
- Start date
Pablo Cruise
Member
Don't say "anti histamine" please, no one maked money on proven old therapies like HCQ.
YourUniverse
Member
Low blood sugar can cause histamine release
- Joined
- Jun 26, 2017
- Messages
- 482
Shortly after a rather severe bout of Covid (un-jabbed), my pulmonologist put me on 40mg famotidine at bedtime for chronic cough. It not only reduced my cough but seems to have helped my recovery. I plan to take it indefinitely as I have no ill effects.
tankasnowgod
Member
- Joined
- Jan 25, 2014
- Messages
- 8,131
This experiment got me thinking...... how did they manage to isolate and purify the "Spike Protein" from SARS-Cov-2, when they never even managed to isolate and purify this "Novel Corona Virus" from the other cellular material when they allegedly "discovered" it in the first place?
The short answer is..... they didn't. The study itself doesn't even make such a claim (contrary to how the title is written). The whole story is told in right here, in the Abstract-
Did you gloss over that word "recombinant?" You shouldn't. It means this is a synthetic protein.
 www.news-medical.net
www.news-medical.net
 en.wikipedia.org
en.wikipedia.org

 www.merriam-webster.com
www.merriam-webster.com
As always, the "Materials and Methods" section gives further detail-
Here is the listing from ProSci-
 www.prosci-inc.com
www.prosci-inc.com
They can claim this synthetic protein is the same as the "Spike Protein" from "SARS-Cov-2, but since neither the alleged virus, nor the alleged spike protein has been isolated and purified, how would anyone possibly know?
Although, since ProSci charges over $500 for 0.1 mg (!!!!), I'm guessing they don't care. And probably prefer no one ask that question.
The short answer is..... they didn't. The study itself doesn't even make such a claim (contrary to how the title is written). The whole story is told in right here, in the Abstract-
Investigating the effects of recombinant SARS-CoV-2 spike protein S1 Receptor-Binding Domain (Spike) on ACE2 expression in cultured human coronary artery endothelial cells, we found that the presence of histamine potentiated spike-mediated ACE2 internalization into endothelial cells.
Did you gloss over that word "recombinant?" You shouldn't. It means this is a synthetic protein.
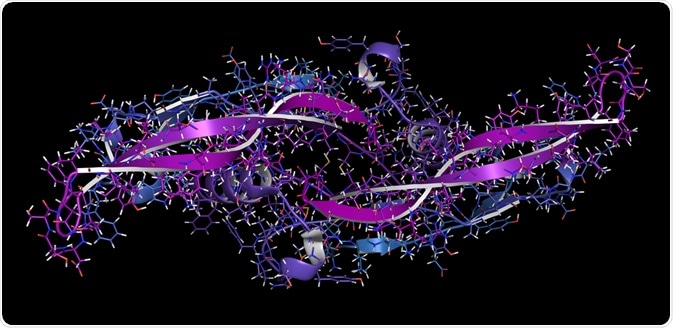
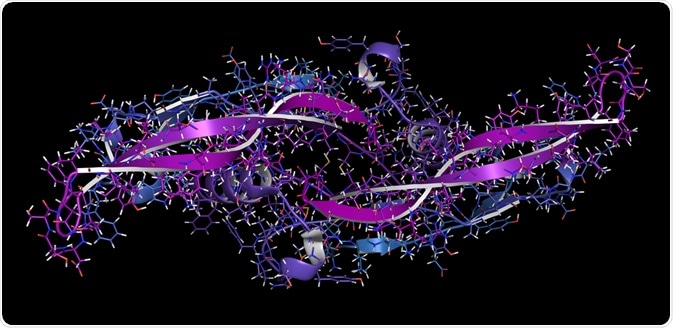
What are Recombinant Proteins?
Recombinant proteins are formed by transfecting foreign genes into a host cell. They are commonly used in the pharmaceutical industry.
Recombinant proteins are formed by transfecting foreign genes into a host cell. Recombinant proteins are commonly used to produce pharmaceutical products, protein-based polymers for drug delivery, antibodies and enzymes for disease treatment, protein scaffolds for tissue engineering, as well as for a myriad of other uses.
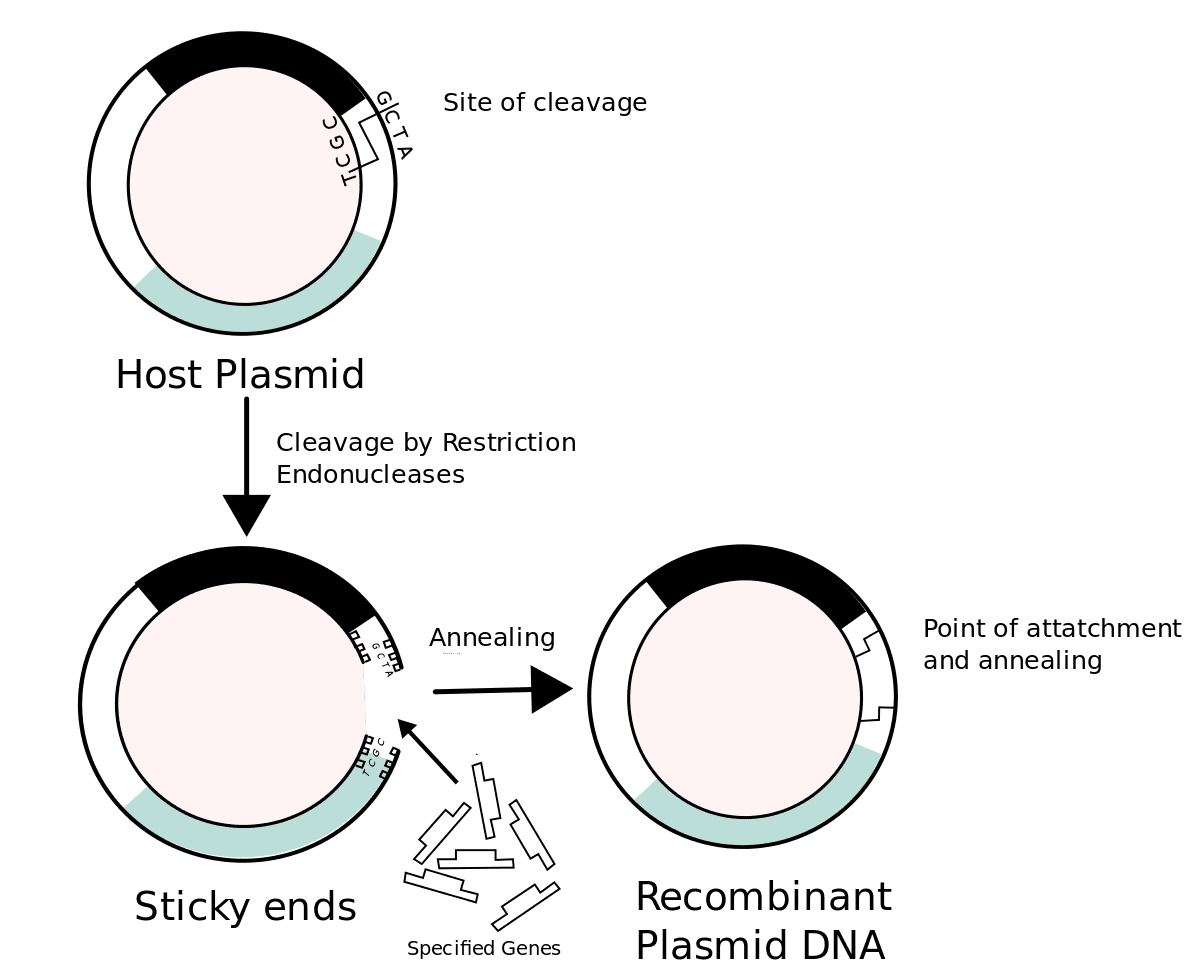
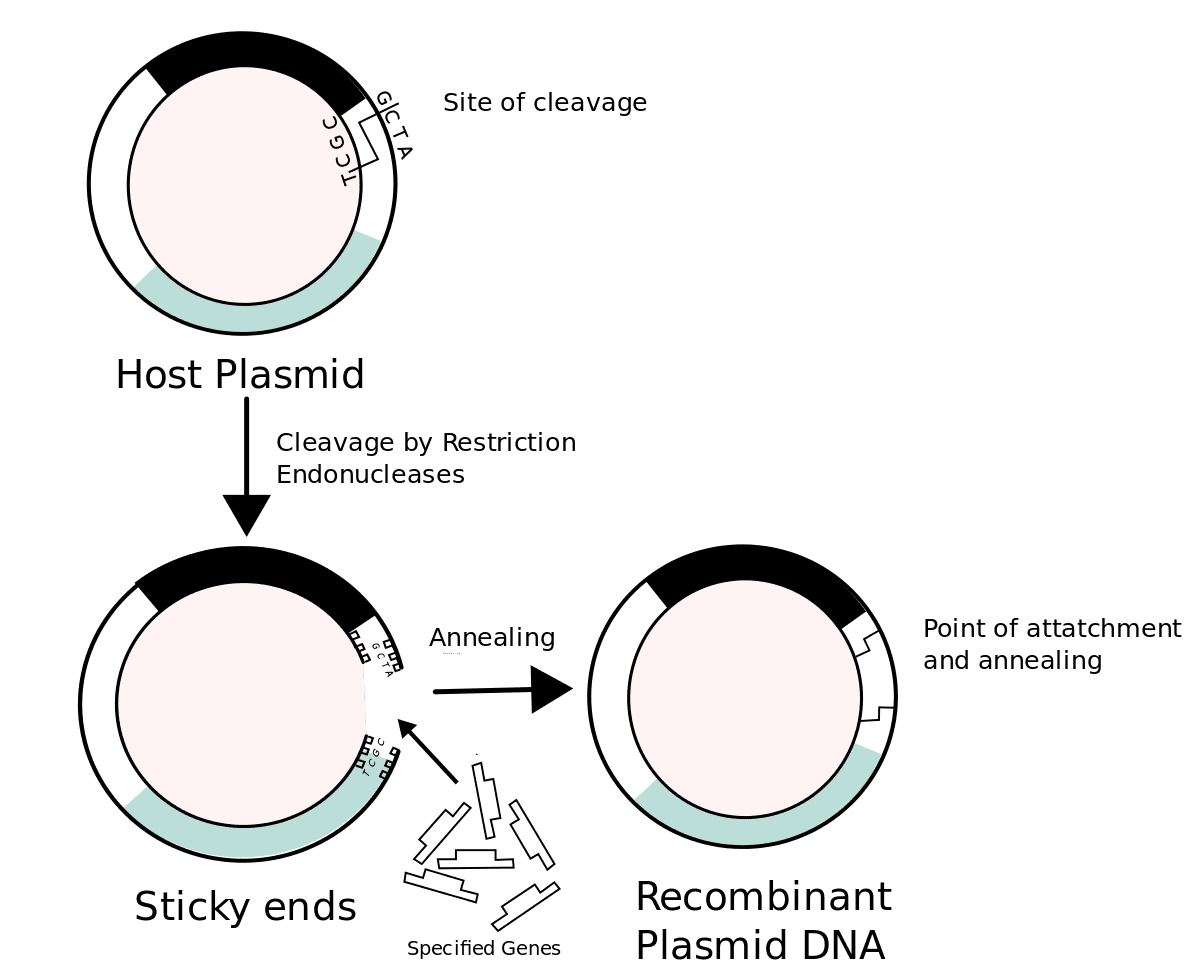
Recombinant DNA - Wikipedia
Recombinant DNA (rDNA) molecules are DNA molecules formed by laboratory methods of genetic recombination (such as molecular cloning) that bring together genetic material from multiple sources, creating sequences that would not otherwise be found in the genome.

Definition of RECOMBINANT
relating to or exhibiting genetic recombination; relating to or containing genetically engineered DNA; produced by genetic engineering… See the full definition
1: relating to or exhibiting genetic recombinationrecombinant progeny
2a: relating to or containing genetically engineered DNA
b: produced by genetic engineering
As always, the "Materials and Methods" section gives further detail-
Cell culture
The human primary coronary artery endothelial cells were purchased from Cell Biologics Inc. The cells were cultured in the endothelial cell medium containing (0.5 ml VEGF, Heparin, EGF, FGF, Hydrocortisone, L-Glutamine, and Antibiotic–Antimycotic Solution) supplemented with 2% fetal bovine serum.
Reagents
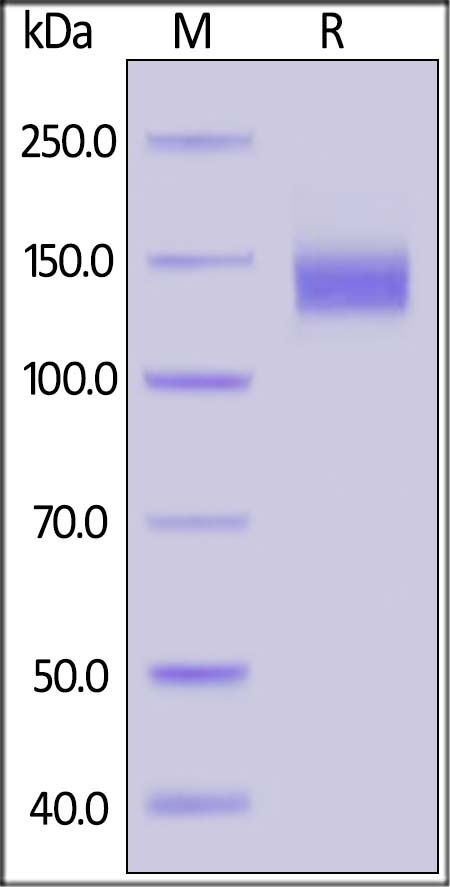
The SARS-CoV-2 (COVID-19) S1 Recombinant Protein (cat. no. 97-092) was purchased from ProSci Inc. (Poway, CA) and used at a final concentration of 10 μg/ml. The endothelial cells were treated with spike protein at the final concentration for the required time before surface biotinylation experiments were carried out. The ACE2 antibody was purchased from Abnova (Taipei, Taiwan, cat. no. PAB13443). Histamine, famotidine, and PKI were purchased from Sigma-Aldrich (St. Louis, MO, United States). siRNA to H2 receptor and scrambled siRNA were purchased from Thermo Fisher Scientific Inc.
Here is the listing from ProSci-
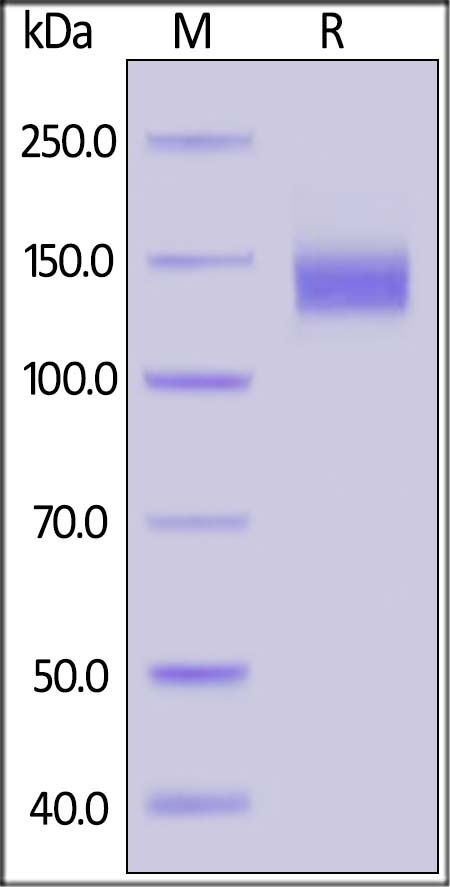
SARS-CoV-2 (COVID-19) S1 Recombinant Protein
SARS-CoV-2 (COVID-19) S1 Recombinant protein - Cat. No. 97-092 | ProSci
They can claim this synthetic protein is the same as the "Spike Protein" from "SARS-Cov-2, but since neither the alleged virus, nor the alleged spike protein has been isolated and purified, how would anyone possibly know?
Although, since ProSci charges over $500 for 0.1 mg (!!!!), I'm guessing they don't care. And probably prefer no one ask that question.
appotis
Member
- Joined
- Jan 10, 2018
- Messages
- 35

Famotidine activates the vagus nerve inflammatory reflex to attenuate cytokine storm - Molecular Medicine
Background Severe COVID-19 is characterized by pro-inflammatory cytokine release syndrome (cytokine storm) which causes high morbidity and mortality. Recent observational and clinical studies suggest famotidine, a histamine 2 receptor (H2R) antagonist widely used to treat gastroesophageal reflux...
Famotidine activates the vagus nerve inflammatory reflex to attenuate cytokine storm
Background
Severe COVID-19 is characterized by pro-inflammatory cytokine release syndrome (cytokine storm) which causes high morbidity and mortality. Recent observational and clinical studies suggest famotidine, a histamine 2 receptor (H2R) antagonist widely used to treat gastroesophageal reflux disease, attenuates the clinical course of COVID-19. Because evidence is lacking for a direct antiviral activity of famotidine, a proposed mechanism of action is blocking the effects of histamine released by mast cells. Here we hypothesized that famotidine activates the inflammatory reflex, a brain-integrated vagus nerve mechanism which inhibits inflammation via alpha 7 nicotinic acetylcholine receptor (α7nAChR) signal transduction, to prevent cytokine storm.
Methods
The potential anti-inflammatory effects of famotidine and other H2R antagonists were assessed in mice exposed to lipopolysaccharide (LPS)-induced cytokine storm. As the inflammatory reflex is integrated and can be stimulated in the brain, and H2R antagonists penetrate the blood brain barrier poorly, famotidine was administered by intracerebroventricular (ICV) or intraperitoneal (IP) routes.
Results
Famotidine administered IP significantly reduced serum and splenic LPS-stimulated tumor necrosis factor (TNF) and IL-6 concentrations, significantly improving survival. The effects of ICV famotidine were significantly more potent as compared to the peripheral route. Mice lacking mast cells by genetic deletion also responded to famotidine, indicating the anti-inflammatory effects are not mast cell-dependent. Either bilateral sub-diaphragmatic vagotomy or genetic knock-out of α7nAChR abolished the anti-inflammatory effects of famotidine, indicating the inflammatory reflex as famotidine’s mechanism of action. While the structurally similar H2R antagonist tiotidine displayed equivalent anti-inflammatory activity, the H2R antagonists cimetidine or ranitidine were ineffective even at very high dosages.
Conclusions
These observations reveal a previously unidentified vagus nerve-dependent anti-inflammatory effect of famotidine in the setting of cytokine storm which is not replicated by high dosages of other H2R antagonists in clinical use. Because famotidine is more potent when administered intrathecally, these findings are also consistent with a primarily central nervous system mechanism of action.
EMF Mitigation - Flush Niacin - Big 5 Minerals
Similar threads
- Replies
- 16
- Views
- 8K
- Replies
- 49
- Views
- 6K
P
- Replies
- 6
- Views
- 4K
- Replies
- 26
- Views
- 5K
P
- Replies
- 10
- Views
- 2K
- Replies
- 6
- Views
- 2K
- Replies
- 0
- Views
- 1K
- Replies
- 0
- Views
- 2K
- Replies
- 8
- Views
- 2K
- Replies
- 14
- Views
- 5K
- Replies
- 8
- Views
- 2K
- Replies
- 4
- Views
- 1K
- Replies
- 7
- Views
- 2K
- Replies
- 0
- Views
- 2K
