pimpnamedraypeat
Member
- Joined
- Dec 25, 2014
- Messages
- 1,045
So why are white people allowed to concede, to strike a deal, and keep their land? Not even the much‐dreaded Germans and Japanese were exterminated after World War II. I think the main reason was: besides looking differently, they were illiterate; they were simply treated as non‐people, or as savages.
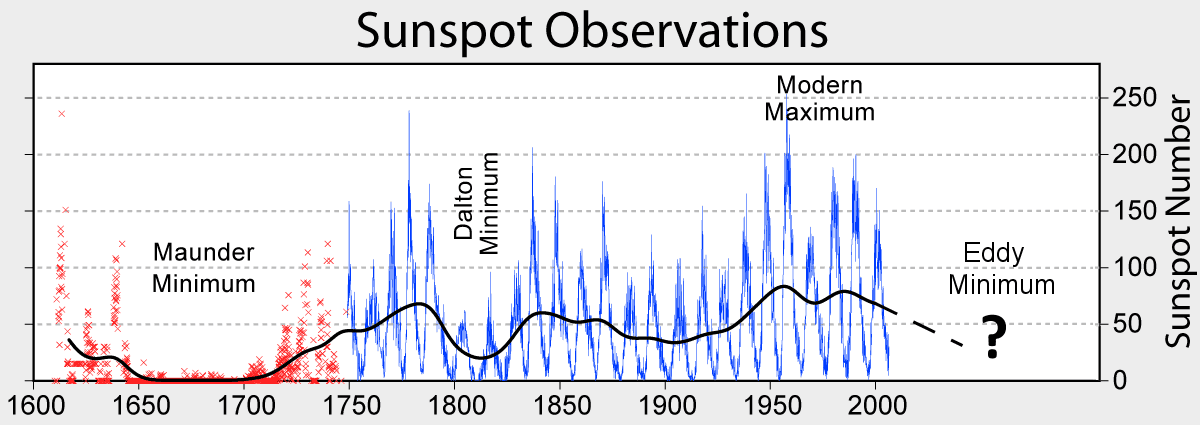
They were needed at the time. The elites don't care for poor whites for anything other than their usefulness. I think in the coming decades we're going to see a large reduction in the human population from war, starvation, and natural disasters. I was researching global warming and stumbled onto the coming ice age. The sun is cooling down and we're going to see a long unending winter that will precipitate a full blown ice age. Human population will drop to approximately georgia guidestone level. Google adapt2030 or not by fire but by ice to learn more
Military men have historically manufactured tension where there'd been none, to increase the public's perception of their trade. Even to this day the public is fed inaccurate reasons for engagement, The Gulf of Tonkin and 9/11 being notable examples, but no doubt it's been occurring for centuries. I think you can be certain even back them, European military men would manufacture lies about the natives to increase the demand for war—and perhaps even staged 'false flag' events. You can also be nearly certain the industrialists also manufactured lies to justify the expropriation of land.
I think this happened a lot. For example scalping was started by the white man (for accounting reasons) but it's now accepted to be a native American tradition.