Hey thanks @Birdie!@Lollipop2 Huba Huba. This is about treatment for Long Covid.
Navigation
Install the app
How to install the app on iOS
Follow along with the video below to see how to install our site as a web app on your home screen.
Note: This feature may not be available in some browsers.
More options
-
By using this site you agree to the terms, rules, and privacy policy.
-
Charlie's Restoration Giveaway #2 (Entire Home EMF Mitigation & Protection Along With Personal Protection) - Click Here To Enter
-
Dear Carnivore Dieters, A Muscle Meat Only Diet is Extremely Healing Because it is a Low "vitamin A" Diet. This is Why it Works so Well...
Rest the rest of this post by clicking here
-
The Forum is transitioning to a subscription-based membership model - Click Here To Read
Click Here if you want to upgrade your account
If you were able to post but cannot do so now, send an email to admin at raypeatforum dot com and include your username and we will fix that right up for you.
You are using an out of date browser. It may not display this or other websites correctly.
You should upgrade or use an alternative browser.
You should upgrade or use an alternative browser.
Microclotting Causing Long COVID
- Thread starter nejdev
- Start date
Ways to fix S1 subunit-infected non-classical monocytes
______
 live.childrenshealthdefense.org
live.childrenshealthdefense.org
Interview of Dr. Ryan Cole by RFK Jr.
August 30, 2021
10:44 --
RFK Jr.: "A lot of our audience has asked me, 'What are doctors doing for long-haul COVID and vaccine injuries... that last for months?'"
Dr. Ryan Cole: "Kudos to Dr. Bruce Patterson, and he has a website, www.covidlonghaulers.com; they're doing research. Mechanistically, there's a certain type of white blood cell -- a non-classical monocyte -- that is still holding fragments of virus and/or spike protein inside of it. It's kind of the same mechanism in the long-hauler and/or the post-COVID patient. Fascinatingly, ivermectin is fantastic for that. For those who have neurologic injury post-vaccine or post-long-haul, fluvoxamine has had great effect in a good percentage of those patients; some patients don't tolerate it, but it's a low dose for a short period of time. I've treated a handful of these individuals -- maybe 16. I would say about 75% of them -- I got this beautiful letter from a gal in New York saying she could barely move, she couldn't function, she couldn't go back to work; after three weeks on treatment she was ecstatic, saying, "I'm 80, 90% better; I'm functional again."
The fluvoxamine is turning off a certain type of white blood cell [infected non-classical monocyte]. Not only those drugs are able to do that. I would encourage people to look at www.flccc.net and look at their I-RECOVER protocols [ I-RECOVER Protocol | FLCCC | Front Line COVID-19 Critical Care Alliance "I-RECOVER Management Protocol for Long Haul COVID-19 Syndrome (LHCS)"]... Vitamin D in good dose will help repolarize and inactivate those non-classical monocytes. One of the statins, atorvastatin, is effective [for infected non-classical monocytes?]. Melatonin, interestingly, because it affects your hormones [is effective for other long-hauler COVID symptoms, I think he means, maybe not for infected non-classical monocytes].
And then there's another line of cells -- your kind of itchy, inflammatory cells -- your mast cells. Some of these patients are hyperactivated in that line of cells, so they can use some antihistamines: famotidine, which is Pepcid, or Claritin allegra, the non-drowsy type."
______
youtube.com/watch?v=JwjJs5ZHKJI
Interview of Dr. Bruce Patterson by Dr. Mobeen Syed
June 24, 2021
6:20 --
Dr. Bruce Patterson: "...non-classical monocytes carry spike protein S1 subunit up to 15 months after diagnosis. These cells bind to blood vessel walls and endothelial cells through fractalkine and the fractalkine receptor that's expressed on non-classical monocytes and cause inflammation, and these cells can cross the blood brain barrier and cause vascular inflammation in the brain. The most exciting thing that we found in the literature... is that these non-classical monocytes are mobilized by exercise and activity. And so here you have a cell carrying spike protein, and no RNA by the way -- we just had a round of sorting experiments and next-gen sequencing... to show that there really isn't any protein in these cells, yet they express the S1 subunit protein. But they are mobilized by exercise, and so of course to a person who's a long-hauler, they get worse after activity, after exercise. We've had individuals who've gotten back to pre-COVID levels, and some individuals who were absolutely bedridden, who felt well enough to work in the yard and take their kids to sporting events and overdid it and had a relapse. The fact is, these cells still contain S1 subunit protein, are still circulating, and a little bit of exercise -- you know, more than just a mile or two walk -- and they're gonna get a flare-up of their symptoms, and that's why you see this waxing and waning. And when we talk about our therapeutic approach, we'll talk about how that can mitigate these flares and eliminate these cells from the circulation."
18:55 --
"We can also interrupt this fractalkine, fractalkine receptor pathway with statins. So the hallmark of our treatment regimen we recommend now is a CCR5 antagonist and statins. And of course, ivermectin, we've found to be very useful in our combinations. We tend not to use it alone because now that we understand the mechanism behind long COVID, we want to interrupt the pathway; we want to treat the cause and not the symptoms. But by no stretch of the imagination do we think ivermectin isn't important in its immunomodulatory effects that complement the CCR5 antagonists and fractalkine...
This has been an important question from our patients: the post-vaccination long-haulers, or the people who've never had [symptomatic] COVID and three or four months after vaccination they have long-hauler symptoms... We found four individuals who had an inflammatory profile that looked a lot like COVID and severe, active COVID, although it wasn't; and the rest look exactly like long-haulers from the long-hauler index... Immunologically, they resemble very much like long-haulers, we've treated them as such, and we've been very successful treating them. As much as it's a side effect of vaccines, I think it's not something to be too concerned about; it's treatable and it's not something that'll stick forever."
22:56 --
"The key point about our discovery is that it's in a highly mobile cell that's in the blood. They're true monocytes -- non-classical monocytes but monocytes nevertheless -- and they have the capacity to go all over your body and cause inflammation..."
25:28 -- "These cells have a definitive lifespan, and if you look at classical monocytes, intermediate monocytes, and non-classical monocytes in normal human beings, you're talking about lifespans of days and weeks. But what happens in pathologic conditions, a whole set of mechanisms that prevent cell death come into play, that make them more long-lived than in normal individuals. That said, using a combination of CCR5 antagonists, statins, and ivermectin, we've seen, by doing serial monitoring of these cells, the levels go down... We've already shown patients in our program who we've got their immune systems back to normal, absolute normal; every one of the cytokines in our panel is normal... Sometimes there's a lag in the symptoms... Usually their symptoms improve right along with their immune profile improving..."
36:15 -- "These non-classical monocytes are expressing CCR5, and much like bees are attracted to honey, these immune cells are attracted to RANTES. And we already showed in our first paper, RANTES are statistically signficantly elevated in long-haulers compared to severe, mild, or moderate, and normal individuals. So, again, RANTES is playing a role in long COVID. It's made by activated platelets, which are probably responding on the inflamed endothelium..."
41:06 --
Dr. Mobeen Syed: "Post-vaccines -- we established that this is happening post-vaccine as well - how is the vaccine ending up causing this?"
Dr. Bruce Patterson: "There's one thing we see that's different from long COVID, and that's the elevations of vascular inflammation markers. The long-hauler index [immune profile]... we don't see the elevations in VEGF, which is great because that causes peripheral neuropathy, and I think it's responsible for the brain fog because those cells cross the blood brain barrier and cause VEGF expression there and vasodilation which is probably the cause of headaches and migraines, but we don't see that [VEGF elevation] in [non-vaccinated?] long-haulers. The most common pattern we see in post-vaccination long-hauler symptoms is RANTES, [also known as] CCL5, plus soluble CD40 ligand in addition to elevations in the long-hauler index... We're going to look in these monocytic subsets, to see in the post-vaccination individuals, if they're still harboring fragments of COVID protein three and four months after vaccination."
Dr. Mobeen Syed: "...Dr. Patterson's team has input on the I-RECOVER protocol on www.flccc.net [ I-RECOVER Protocol | FLCCC | Front Line COVID-19 Critical Care Alliance ]."
50:22 --
Dr. Mobeen Syed: "...What is the relationship of tinnitus with this mechanism?"
Dr. Bruce Patterson: "We very often see tinnitus with brain fog, and what's really miraculous is that I'd say within 3-5 days tinnitus is gone with a CCR5 antagonist... I'm thinking that preventing the migration of cells, at least in long-haulers, into the brain, and preventing vasodilation, which I think is part and parcel with tinnitus and increased pressure in certain parts of the brain -- we see tinnitus a lot, we treat it a lot, and I think we're very good at eliminating it."
My worry is that with the long-haulers, when there is a continuous inflammation going on, and now thanks to your work we know that it is at the boundaries of the blood vessels and vasculitis is occurring, there could be damage if this continues on for a long time because there could be scarring on top of the damage and that can become a permanent issue. And so that means that managing this as fast as possible becomes an important issue... to prevent scarring."
_____
Using nicotine to cause apoptosis of S1 subunit-infected monocytes

 forum.jackkruse.com
forum.jackkruse.com
______
‘The Defender Show’ Season 1, Episode 9: Frontline Healer — Dr. Ryan Cole - The Defender Show - CHD TV: Livestreaming Video & Audio
Live events, weekly shows, educational videos and podcasts.
Interview of Dr. Ryan Cole by RFK Jr.
August 30, 2021
10:44 --
RFK Jr.: "A lot of our audience has asked me, 'What are doctors doing for long-haul COVID and vaccine injuries... that last for months?'"
Dr. Ryan Cole: "Kudos to Dr. Bruce Patterson, and he has a website, www.covidlonghaulers.com; they're doing research. Mechanistically, there's a certain type of white blood cell -- a non-classical monocyte -- that is still holding fragments of virus and/or spike protein inside of it. It's kind of the same mechanism in the long-hauler and/or the post-COVID patient. Fascinatingly, ivermectin is fantastic for that. For those who have neurologic injury post-vaccine or post-long-haul, fluvoxamine has had great effect in a good percentage of those patients; some patients don't tolerate it, but it's a low dose for a short period of time. I've treated a handful of these individuals -- maybe 16. I would say about 75% of them -- I got this beautiful letter from a gal in New York saying she could barely move, she couldn't function, she couldn't go back to work; after three weeks on treatment she was ecstatic, saying, "I'm 80, 90% better; I'm functional again."
The fluvoxamine is turning off a certain type of white blood cell [infected non-classical monocyte]. Not only those drugs are able to do that. I would encourage people to look at www.flccc.net and look at their I-RECOVER protocols [ I-RECOVER Protocol | FLCCC | Front Line COVID-19 Critical Care Alliance "I-RECOVER Management Protocol for Long Haul COVID-19 Syndrome (LHCS)"]... Vitamin D in good dose will help repolarize and inactivate those non-classical monocytes. One of the statins, atorvastatin, is effective [for infected non-classical monocytes?]. Melatonin, interestingly, because it affects your hormones [is effective for other long-hauler COVID symptoms, I think he means, maybe not for infected non-classical monocytes].
And then there's another line of cells -- your kind of itchy, inflammatory cells -- your mast cells. Some of these patients are hyperactivated in that line of cells, so they can use some antihistamines: famotidine, which is Pepcid, or Claritin allegra, the non-drowsy type."
______
youtube.com/watch?v=JwjJs5ZHKJI
Interview of Dr. Bruce Patterson by Dr. Mobeen Syed
June 24, 2021
6:20 --
Dr. Bruce Patterson: "...non-classical monocytes carry spike protein S1 subunit up to 15 months after diagnosis. These cells bind to blood vessel walls and endothelial cells through fractalkine and the fractalkine receptor that's expressed on non-classical monocytes and cause inflammation, and these cells can cross the blood brain barrier and cause vascular inflammation in the brain. The most exciting thing that we found in the literature... is that these non-classical monocytes are mobilized by exercise and activity. And so here you have a cell carrying spike protein, and no RNA by the way -- we just had a round of sorting experiments and next-gen sequencing... to show that there really isn't any protein in these cells, yet they express the S1 subunit protein. But they are mobilized by exercise, and so of course to a person who's a long-hauler, they get worse after activity, after exercise. We've had individuals who've gotten back to pre-COVID levels, and some individuals who were absolutely bedridden, who felt well enough to work in the yard and take their kids to sporting events and overdid it and had a relapse. The fact is, these cells still contain S1 subunit protein, are still circulating, and a little bit of exercise -- you know, more than just a mile or two walk -- and they're gonna get a flare-up of their symptoms, and that's why you see this waxing and waning. And when we talk about our therapeutic approach, we'll talk about how that can mitigate these flares and eliminate these cells from the circulation."
18:55 --
"We can also interrupt this fractalkine, fractalkine receptor pathway with statins. So the hallmark of our treatment regimen we recommend now is a CCR5 antagonist and statins. And of course, ivermectin, we've found to be very useful in our combinations. We tend not to use it alone because now that we understand the mechanism behind long COVID, we want to interrupt the pathway; we want to treat the cause and not the symptoms. But by no stretch of the imagination do we think ivermectin isn't important in its immunomodulatory effects that complement the CCR5 antagonists and fractalkine...
This has been an important question from our patients: the post-vaccination long-haulers, or the people who've never had [symptomatic] COVID and three or four months after vaccination they have long-hauler symptoms... We found four individuals who had an inflammatory profile that looked a lot like COVID and severe, active COVID, although it wasn't; and the rest look exactly like long-haulers from the long-hauler index... Immunologically, they resemble very much like long-haulers, we've treated them as such, and we've been very successful treating them. As much as it's a side effect of vaccines, I think it's not something to be too concerned about; it's treatable and it's not something that'll stick forever."
22:56 --
"The key point about our discovery is that it's in a highly mobile cell that's in the blood. They're true monocytes -- non-classical monocytes but monocytes nevertheless -- and they have the capacity to go all over your body and cause inflammation..."
25:28 -- "These cells have a definitive lifespan, and if you look at classical monocytes, intermediate monocytes, and non-classical monocytes in normal human beings, you're talking about lifespans of days and weeks. But what happens in pathologic conditions, a whole set of mechanisms that prevent cell death come into play, that make them more long-lived than in normal individuals. That said, using a combination of CCR5 antagonists, statins, and ivermectin, we've seen, by doing serial monitoring of these cells, the levels go down... We've already shown patients in our program who we've got their immune systems back to normal, absolute normal; every one of the cytokines in our panel is normal... Sometimes there's a lag in the symptoms... Usually their symptoms improve right along with their immune profile improving..."
36:15 -- "These non-classical monocytes are expressing CCR5, and much like bees are attracted to honey, these immune cells are attracted to RANTES. And we already showed in our first paper, RANTES are statistically signficantly elevated in long-haulers compared to severe, mild, or moderate, and normal individuals. So, again, RANTES is playing a role in long COVID. It's made by activated platelets, which are probably responding on the inflamed endothelium..."
41:06 --
Dr. Mobeen Syed: "Post-vaccines -- we established that this is happening post-vaccine as well - how is the vaccine ending up causing this?"
Dr. Bruce Patterson: "There's one thing we see that's different from long COVID, and that's the elevations of vascular inflammation markers. The long-hauler index [immune profile]... we don't see the elevations in VEGF, which is great because that causes peripheral neuropathy, and I think it's responsible for the brain fog because those cells cross the blood brain barrier and cause VEGF expression there and vasodilation which is probably the cause of headaches and migraines, but we don't see that [VEGF elevation] in [non-vaccinated?] long-haulers. The most common pattern we see in post-vaccination long-hauler symptoms is RANTES, [also known as] CCL5, plus soluble CD40 ligand in addition to elevations in the long-hauler index... We're going to look in these monocytic subsets, to see in the post-vaccination individuals, if they're still harboring fragments of COVID protein three and four months after vaccination."
Dr. Mobeen Syed: "...Dr. Patterson's team has input on the I-RECOVER protocol on www.flccc.net [ I-RECOVER Protocol | FLCCC | Front Line COVID-19 Critical Care Alliance ]."
50:22 --
Dr. Mobeen Syed: "...What is the relationship of tinnitus with this mechanism?"
Dr. Bruce Patterson: "We very often see tinnitus with brain fog, and what's really miraculous is that I'd say within 3-5 days tinnitus is gone with a CCR5 antagonist... I'm thinking that preventing the migration of cells, at least in long-haulers, into the brain, and preventing vasodilation, which I think is part and parcel with tinnitus and increased pressure in certain parts of the brain -- we see tinnitus a lot, we treat it a lot, and I think we're very good at eliminating it."
My worry is that with the long-haulers, when there is a continuous inflammation going on, and now thanks to your work we know that it is at the boundaries of the blood vessels and vasculitis is occurring, there could be damage if this continues on for a long time because there could be scarring on top of the damage and that can become a permanent issue. And so that means that managing this as fast as possible becomes an important issue... to prevent scarring."
_____
Using nicotine to cause apoptosis of S1 subunit-infected monocytes
Another relatively easy article on prions...
Gotu kola (centella asiatica)' and brahmi (bacopa monnieri) are each called a medhya rasayana -- translates to ~ brain/nerves restorative. Medhya...
 forum.jackkruse.com
forum.jackkruse.com
Discovery of Novel GPVI Receptor Antagonists by Structure-Based Repurposing
Inappropriate platelet aggregation creates a cardiovascular risk that is largely managed with thienopyridines and aspirin. Although effective, these drugs carry risks of increased bleeding and drug ‘resistance’, underpinning a drive for new antiplatelet agents. To discover such drugs, one strategy is to identify a suitable druggable target and then find small molecules that modulate it. A good and unexploited target is the platelet collagen receptor, GPVI, which promotes thrombus formation. To identify inhibitors of GPVI that are safe and bioavailable, we docked a FDA-approved drug library into the GPVI collagen-binding site in silico. We now report that losartan and cinanserin inhibit GPVI-mediated platelet activation in a selective, competitive and dose-dependent manner. This mechanism of action likely underpins the cardioprotective effects of losartan that could not be ascribed to its antihypertensive effects. We have, therefore, identified small molecule inhibitors of GPVI-mediated platelet activation, and also demonstrated the utility of structure-based repurposing.
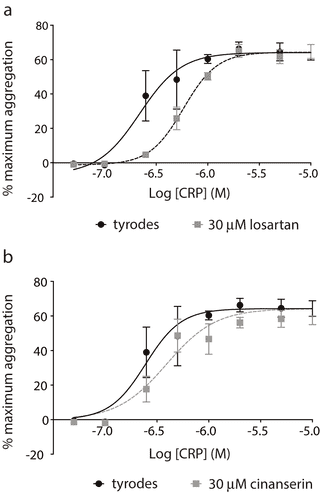
 journals.plos.org
journals.plos.org
Inappropriate platelet aggregation creates a cardiovascular risk that is largely managed with thienopyridines and aspirin. Although effective, these drugs carry risks of increased bleeding and drug ‘resistance’, underpinning a drive for new antiplatelet agents. To discover such drugs, one strategy is to identify a suitable druggable target and then find small molecules that modulate it. A good and unexploited target is the platelet collagen receptor, GPVI, which promotes thrombus formation. To identify inhibitors of GPVI that are safe and bioavailable, we docked a FDA-approved drug library into the GPVI collagen-binding site in silico. We now report that losartan and cinanserin inhibit GPVI-mediated platelet activation in a selective, competitive and dose-dependent manner. This mechanism of action likely underpins the cardioprotective effects of losartan that could not be ascribed to its antihypertensive effects. We have, therefore, identified small molecule inhibitors of GPVI-mediated platelet activation, and also demonstrated the utility of structure-based repurposing.
Discovery of Novel GPVI Receptor Antagonists by Structure-Based Repurposing
Inappropriate platelet aggregation creates a cardiovascular risk that is largely managed with thienopyridines and aspirin. Although effective, these drugs carry risks of increased bleeding and drug ‘resistance’, underpinning a drive for new antiplatelet agents. To discover such drugs, one...
This would be the same interview that 863127 posted the transcript for. Helpful to have the transcript. Thank you.Hey thanks @Birdie!
"McCullough uses full-dose aspirin — 325 milligrams a day — in almost everyone with long COVID syndrome who doesn’t have a major blood clot, in addition to other medications."
How to Manage Long-Haul Syndrome (48 hrs or less to view and download)
How to Manage Long-Haul Syndrome (48 hrs or less to view and download)
Thanks for this."McCullough uses full-dose aspirin — 325 milligrams a day — in almost everyone with long COVID syndrome who doesn’t have a major blood clot, in addition to other medications."
How to Manage Long-Haul Syndrome (48 hrs or less to view and download)
Lots of good responses here folks. Thanks so much for contributing. Taking some time to get through all of this.
I have been to the "post COVID clinic" here in Scandinavia. They didn't have much to offer. The infectious disease doctor that I met with told me that she thinks one of the main causes of long haul COVID is nerve damage...she said she thinks the microglial cells which nourish nerve cells get damaged, and so the parasympathetic and sympathetic nervous system components go crazy. This could be one of the causes. She gave me a prescription for amitriptyline which is supposed to help me sleep, but I haven't taken it yet. I actually wonder if it would work for my long haul the same way that fluvoxamine has been purported to, but I am extremely leary of taking any pharmaceuticals. I tried ivermectin and got some weird side effects, but it temporarily reduced inflammation which is why I think they say it cures long haul. I don't think it's curing anything, I think it's just a good anti-inflammatory. Soon as you stop, the symptoms come back. I've had this happen, many others as well.
I've had a brain MRI, xray of my lungs, EKG/blood work for heart and everything else - all my tests are coming back normal. At this point, I'm not sure what the hell is going on. I have seem *some* small improvements over the past 10 months but it's very slow going. Will continue to report in.
Thanks again for all this information, great stuff.
I have been to the "post COVID clinic" here in Scandinavia. They didn't have much to offer. The infectious disease doctor that I met with told me that she thinks one of the main causes of long haul COVID is nerve damage...she said she thinks the microglial cells which nourish nerve cells get damaged, and so the parasympathetic and sympathetic nervous system components go crazy. This could be one of the causes. She gave me a prescription for amitriptyline which is supposed to help me sleep, but I haven't taken it yet. I actually wonder if it would work for my long haul the same way that fluvoxamine has been purported to, but I am extremely leary of taking any pharmaceuticals. I tried ivermectin and got some weird side effects, but it temporarily reduced inflammation which is why I think they say it cures long haul. I don't think it's curing anything, I think it's just a good anti-inflammatory. Soon as you stop, the symptoms come back. I've had this happen, many others as well.
I've had a brain MRI, xray of my lungs, EKG/blood work for heart and everything else - all my tests are coming back normal. At this point, I'm not sure what the hell is going on. I have seem *some* small improvements over the past 10 months but it's very slow going. Will continue to report in.
Thanks again for all this information, great stuff.
Texon
Member
- Joined
- Nov 28, 2016
- Messages
- 671
I agree with you. Lots going on with this we don't have a clue about yet.I
I never said I just KNOW. I’m dealing with what’s more likely. I think what’s likely is that COVID was produced in a lab and released. Could I be wrong? Sure. Could I be sick with some other weird ailment? Sure. But what I’m thinking is more likely is that there was a pandemic engineered to get people vaccinated. Ive seen the receipts from the NIH making payments to Wuhan Institute of Virology for coronavirus “research” (usaspending.gov) and read the FOIA info where they literally propose making chimeric viruses based off the bat flu. So, yeah. I’m gonna go out on a limb and say that me, who’s been perfectly healthy my whole life and hasn’t really changed his routine much, caught something “not natural”, just like many, many other folks.
I have tried Famotidin and I still take it. I use both H1 and H2 blockers to block histamine. So usually I cycle between desloratadine and Famotidin for maximum benefit.
As for serotonin, I can’t make any definite assumptions about that. But I can say that I haven’t been isolated. We live in Sweden now. There was barely a “lockdown”. Things are pretty much normal around here, ironically. So not sure if my body suddenly decided to ramp up serotonin production and hence blood clots. Not saying it’s impossible, just don’t see a cause/effect pattern that you mentioned.
ddjd
Member
- Joined
- Jul 13, 2014
- Messages
- 6,722
EMF Mitigation - Flush Niacin - Big 5 Minerals
Similar threads
- Replies
- 13
- Views
- 2K
- Replies
- 81
- Views
- 22K
- Replies
- 11
- Views
- 4K
- Replies
- 149
- Views
- 19K
P
- Replies
- 2
- Views
- 2K
- Replies
- 153
- Views
- 20K
- Replies
- 76
- Views
- 5K
- Replies
- 16
- Views
- 8K
- Replies
- 8
- Views
- 2K
- Replies
- 7
- Views
- 3K
- Replies
- 55
- Views
- 11K
P
