Travis
Member
- Joined
- Jul 14, 2016
- Messages
- 3,189
Mast cells travel to the brain and have been estimated to be the major source of brain histamine in people who have them. The range varies considerably: histologists have counted thousands in some people, and zero in others. These can be induced by immunogenic peptides derived from food, and also can be induced by ionizing radiation. Histamine is neurotransmitter proper. Normal brain histamine is created not from mast cells, but by the tuberomammillary nucleus—a brain structure which can be seen as analogous to the serotonergic raphe nucleus; and like the raphe nucleus, the tuberomammillary nucleus sends centimetre‐long projections throughout.
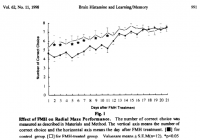
Brain histamine has consistently been shown to reduce learning in rats. Brain histamine is a stimulant, a property not necessarily in contradiction to its effects on learning. While it's true that other stimulants—such as nicotine, acetylcholine, and glutamate—promote learning, I can't think of a fundamental reason why a stimulant must promote memory consolidation (especially considering the weight of evidence which suggests otherwise):
Mast cells have unique properties which allow localization, and are counted on the microscope by histologists. It would be—of course—impossible to count them all yet histologists ostensibly have the patience, discipline, and posture to count to over one thousand:
Imagine the histologists relief upon seeing a brain with no mast cells. What is good for the histologist is good for the subject—that is to say before, when they were still alive.
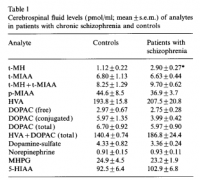
Total mast cell numbers exhibit great interpersonal variation, and does psychology. There has been a convincing histaminergic theory of schizophrenia proposed (Heleniak, 1999), risk ratios of ~4 have been found between celiac disease and schizophrenia (Kalaydjian, 2005), mast cells in the celiac intestine have been found elevated approximately threefold over controls (Strobel, 1983), and histamine has actually been detected the brain of schizophrenics at levels 2.6 that of controls (Prell, 1995). Such findings might suggest that it's actually the histamine that is doing this, and not oft‐speculated gluten exorphin also perennially found elevated in the cerebospinal fluid of patients diagnosed with same condition (Dohan, 1988). But this conflicting theory only strengthens the histaminergic one, since gluten exorphins in the brain are both indicative of current wheat consumption and also the inability of the subject to completely hydrolyze the proline‐rich peptides found therein—both prerequisites for an immunogenic reaction to gluten.

In the year 1985 Robert C. Goldschmidt counted mast cells in the rat brain, and had also determined the histamine content of the same brains. His experiment provided the data necessary to correlate mast cells and brain histamine. He drew two distinctions, and had made two separate correlations: thalmic histamine vs mast cells, and whole brain histamine vs mast cells.

Mast cells are migratory cells, induced by both by immunogenic stimulation and radiation (Ibrahim, 1973). These have been shown capable of migrating to the brain where they can contribute up to 90% of total histamine. Of course, none of this would matter if histamine was totally benign—but it's not!
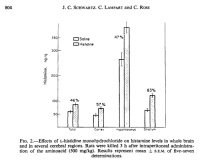
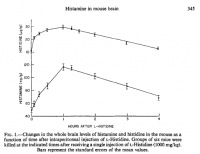
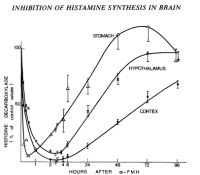
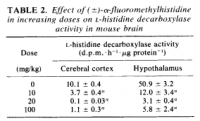
Histamine decreases learning in various rat models measured in various ways, differing both in method of histaminergic manipulation and mnemonic metric. The simplest and straightforward is, of course, raising histamine directly; this can be done either by intracranial injection or the serological delivery of amino acid histidine via injection or ingestion; histamine synthesis from serum histadine follows Fernstrom‐like serotonin/tryptophan kinetics, having appreciable brain uptake while also being liable to the influence competing amino acids—a different set in the case of histidine (Taylor, 1972; Schwarz, 1971).
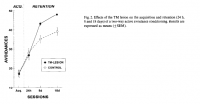
In the most direct type of experiment, histamine is applied directly to the brain via cannula (Eidi, 2003). The use of control rats eliminates the possibility that trauma has anything to do with this, since the same surgery is given to both; control rats were also administered saline in this study. As a result of direct histamine application and passive avoidance electric foot‐shock trials, it had been determined that histamine is a detriment to learning:
'The present data show that scopolamine, the muscarinic receptor antagonist, potentiates the histamine-induced decrease of memory retention, while the histamine receptor antagonists, pyrilamine and cimetidine, increased the acetylcholine- or nicotine-induced enhancement, but attenuated the inhibitory response induced by scopolamine.' ―Eidi
Histadine antagonizes both nicotine and acetylcholine; the converse is also true. This could be the reason why schizophrenics smoke more often than the general population (de Leon, 2005); they could be using nicotine as a device to counteract gluten‐induced mast cell histamine. The odds ratio between schizophrenia and smoking was found to be 5.9×, similar to the ~4× risk ratios between schizophrenia and gluten (and the ~3× elevated intestinal mast cells in celiacs). I do remember—over ten years ago after not having eaten gluten for months—I had found myself to be nearly chain‐smoking Nat Sherman MCDs in an attempt to ward‐off the lobotomizing effects I felt impinging on my brain which had incurred after eating wheatbread during an acute money‐deficiency. Perhaps it was the exorphins, but perhaps the histamine. Gluten peptides have been shown, like cortisol, to release histamine from mast cells as well as induce them.
Brain histamine has consistently been shown to reduce learning in rats. Brain histamine is a stimulant, a property not necessarily in contradiction to its effects on learning. While it's true that other stimulants—such as nicotine, acetylcholine, and glutamate—promote learning, I can't think of a fundamental reason why a stimulant must promote memory consolidation (especially considering the weight of evidence which suggests otherwise):
Persinger, Michael A. "Mast cells in the brain: possibilities for physiological psychology." Physiological Psychology (1977)
Mast cells have unique properties which allow localization, and are counted on the microscope by histologists. It would be—of course—impossible to count them all yet histologists ostensibly have the patience, discipline, and posture to count to over one thousand:
'Dropp's (1976, personal communication) latest investigations involved normal brains from 103 human subjects between 1 and 98 years of age. MCs were found only in the infundibulum, pineal body, area postrema, and supraoptic crest; four of the individuals demonstrated MCs within the subfornical organ while another three subjects showed MCs attached to choroid plexuses within the ventricles. Again large ranges in cell numbers were encountered. MCs within the adult pineal body ranged from only a few to 49,000, while those in the infundibulum ranged from 0 to 7,000.' ―Persinger
'The laboratory rat demonstrates a similar marked intraspecies variation. Total brain MCs ranged between 333 and 4,358 in 10 hooded rats and between 632 and 1,205 in 3 albino rats.' ―Persinger
'Dropp (1972, 1976) reported between 0 and 1,500 total MC numbers within the brains of squirrel monkeys, but found no brain MCs within five mulatta monkeys; three chimpanzees displayed 8,600, 15,470 and 69,570 total brain MCs. Thirteen cat brains analyzed by Dropp (1974) displayed total MCs ranging from 144 to 203,226.' ―Persinger
Imagine the histologists relief upon seeing a brain with no mast cells. What is good for the histologist is good for the subject—that is to say before, when they were still alive.
Total mast cell numbers exhibit great interpersonal variation, and does psychology. There has been a convincing histaminergic theory of schizophrenia proposed (Heleniak, 1999), risk ratios of ~4 have been found between celiac disease and schizophrenia (Kalaydjian, 2005), mast cells in the celiac intestine have been found elevated approximately threefold over controls (Strobel, 1983), and histamine has actually been detected the brain of schizophrenics at levels 2.6 that of controls (Prell, 1995). Such findings might suggest that it's actually the histamine that is doing this, and not oft‐speculated gluten exorphin also perennially found elevated in the cerebospinal fluid of patients diagnosed with same condition (Dohan, 1988). But this conflicting theory only strengthens the histaminergic one, since gluten exorphins in the brain are both indicative of current wheat consumption and also the inability of the subject to completely hydrolyze the proline‐rich peptides found therein—both prerequisites for an immunogenic reaction to gluten.
'A report by Hadjivassiliou et al. (15) showed that 57% of patients with neurological dysfunction of unknown cause had serological evidence of gluten sensitivity in contrast to the control rate of only 12%.' ―Kalaydjian
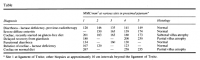
Strobel, S. "Human intestinal mucosal mast cells: expanded population in untreated coeliac disease." Gut (1983) [right image]
Prell, George D. "Histamine metabolites in cerebrospinal fluid of patients with chronic schizophrenia: their relationships to levels of other aminergic transmitters and ratings of symptoms." Schizophrenia research (1995) [left image]
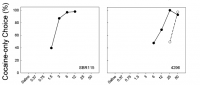
Mast cells travel to the brain a fact which has been proven in two separate rat studies—at minimum. The way this had been proven was through the use of a green fluorescent dye to stain mast cells ex vivo—using chloromethylfluorescein diacetate, which is incorporated into the cell and trapped—with these same labeled green cells being then injected afterwords into a living, and rather furry, rat. Mast cells also contain tryptophan which absorbs blue light strongly, resulting a red reflection when viewed under many lighting conditions. Bombarding the cell with blue, or near ultraviolet, light results in dim tryptophan (since most blue light is absorbed) but the characteristic green of chloromethylfluorescein emitting at 520λ is apparent. The superposition of the two images or course makes yellow; but more importantly, this proves that mast cells migrate into the brain:Prell, George D. "Histamine metabolites in cerebrospinal fluid of patients with chronic schizophrenia: their relationships to levels of other aminergic transmitters and ratings of symptoms." Schizophrenia research (1995) [left image]
Silverman, Ann-Judith. "Mast cells migrate from blood to brain." Journal of Neuroscience (2000)
In the year 1985 Robert C. Goldschmidt counted mast cells in the rat brain, and had also determined the histamine content of the same brains. His experiment provided the data necessary to correlate mast cells and brain histamine. He drew two distinctions, and had made two separate correlations: thalmic histamine vs mast cells, and whole brain histamine vs mast cells.
'These results are direct biochemical evidence for a contribution by MCs to brain HA levels, and indicate that thalamic MCs contribute up to 90% of the HA in thalamus, and up to 50% of whole brain HA levels.' ―Goldschmidt
'The significant correlations between MC numbers and thalamic HA levels (Fig. 2) also provide a method to estimate directly the amount of brain HA contributed by MCs. Thus, without making any assumptions about other stores of thalamic HA, the y-intercepts of the regression lines of Fig. 2 are suggestive of the mean thalamic HA levels in the absence of MCs (6.8 and 8.5 ng for males and females, respectively). With these values for non‐MC histamine, the ranges of thalamic HA values found (Fig. 2) suggest that thalamic MCs contribute a mean of 81% (0-92%) and 54% (0-82%) of the thalamic HA in males and females, respectively. Similarly, the slopes of these regression lines provide estimates of the mean HA content per MC, i.e., 2.5 and 1.3 pg/cell, for males and females, respectively.' ―Goldschmidt
Also found by Goldschmidt was that range of values, going from zero to thousands. At 2.5 picograms histamine per mast cell, this can contribute up to 90% of total brain histamine in some rats. The correlation between mast cells and brain histamine was very good, what you'd rightly expect from more mast cells—migrating immunogenic cells known specifically for releasing histamine, much more than they are known for anything else.
'Thalamic HA content was significantly correlated with the estimated thalamic MC numbers both in males (r = 0.843) and in females (r = 0.678).' ―Goldschmidt

'Individual levels ranged over more than an order of magnitude in both sexes (males: 89–1, 138 ng/g; females: 60–596 ng/g). Whole brain levels were 58 ± 3 ng/g in males (33–89 ng/g) and 54 ± 3 ng/g in females (37–84 ng/g, Table I), not significantly different' ―Goldschmidt
Mast cells are migratory cells, induced by both by immunogenic stimulation and radiation (Ibrahim, 1973). These have been shown capable of migrating to the brain where they can contribute up to 90% of total histamine. Of course, none of this would matter if histamine was totally benign—but it's not!
Goldschmidt, Robert C. "Rat brain mast cells: contribution to brain histamine levels." Journal of neurochemistry (1985)
Histamine decreases learning in various rat models measured in various ways, differing both in method of histaminergic manipulation and mnemonic metric. The simplest and straightforward is, of course, raising histamine directly; this can be done either by intracranial injection or the serological delivery of amino acid histidine via injection or ingestion; histamine synthesis from serum histadine follows Fernstrom‐like serotonin/tryptophan kinetics, having appreciable brain uptake while also being liable to the influence competing amino acids—a different set in the case of histidine (Taylor, 1972; Schwarz, 1971).
'The intraperitoneal administration of L-histidine in a dose of 1000 mg/kg increased threefold the whole brain levels of histamine in the mouse. This increase was evident in all brain regions except the medulla oblongata-pons.' ―Taylor
'Administration of L-histidine at the rate of 500 mg/kg induced an increase of nearly 50 per cent in the level of histamine in rat brain which lasted several hours.' ―Schwarz
Although protein ratios would be expected to alter brain histidine levels, the production capacity of mast cells would likely overshadow subtle dietary manipulations. Worrying about the His/Σ(cAA) ratio while having mast cells present in the brain would be tantamount to worrying about Joey's dilemma with Phoebe—from the television program Friends—while you're house is on fire. Perhaps those on a totally hypoimmunogenic diet could worry about such things, but considering how vitally important histidine is it probably shouldn't be greatly diminished. Histidine is necessary to chelate zinc and transport it throughout the body, is used as a structural component for newly‐synthesized proteins, and also becomes urocanic acid—an ultraviolet light‐absorbing molecule of the skin which protects against sun damage. 'Administration of L-histidine at the rate of 500 mg/kg induced an increase of nearly 50 per cent in the level of histamine in rat brain which lasted several hours.' ―Schwarz
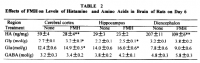
In the most direct type of experiment, histamine is applied directly to the brain via cannula (Eidi, 2003). The use of control rats eliminates the possibility that trauma has anything to do with this, since the same surgery is given to both; control rats were also administered saline in this study. As a result of direct histamine application and passive avoidance electric foot‐shock trials, it had been determined that histamine is a detriment to learning:
'Further analysis showed that post-training injections of histamine or scopolamine decreased memory retention, and lower doses of the two drugs, which did not elicit any response by themselves, showed inhibition of memory retention.' ―Eidi
'Our data indicate that the memory improvement induced by acetylcholine or nicotine can be impaired by histamine.
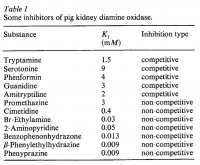
Cimetidine is the classic histamine antagonist, and this too was used. Nicotine and acetylcholine are nearly functionally synonymous, and work to the same end on the nicotinic acetylcholine receptor. These two drugs have long been proven to facilitate things like word recall, reaction time, and attention. The drugs scopolamine (used) and atropine (not used) are the classic muscarinic receptor antagonists. Perhaps most noteworthy is the fact that cimetidine, a histamine antagonist, increased learning.
'The present data show that scopolamine, the muscarinic receptor antagonist, potentiates the histamine-induced decrease of memory retention, while the histamine receptor antagonists, pyrilamine and cimetidine, increased the acetylcholine- or nicotine-induced enhancement, but attenuated the inhibitory response induced by scopolamine.' ―Eidi
'Administration of histamine (5–20 μg/rat) reduced, but the histamine H₁ receptor antagonist, pyrilamine (10–50 μg/rat), and the histamine H₂ receptor antagonist, cimetidine (1–50 μg/rat), increased memory retention in rats.' ―Eidi
Histadine antagonizes both nicotine and acetylcholine; the converse is also true. This could be the reason why schizophrenics smoke more often than the general population (de Leon, 2005); they could be using nicotine as a device to counteract gluten‐induced mast cell histamine. The odds ratio between schizophrenia and smoking was found to be 5.9×, similar to the ~4× risk ratios between schizophrenia and gluten (and the ~3× elevated intestinal mast cells in celiacs). I do remember—over ten years ago after not having eaten gluten for months—I had found myself to be nearly chain‐smoking Nat Sherman MCDs in an attempt to ward‐off the lobotomizing effects I felt impinging on my brain which had incurred after eating wheatbread during an acute money‐deficiency. Perhaps it was the exorphins, but perhaps the histamine. Gluten peptides have been shown, like cortisol, to release histamine from mast cells as well as induce them.
Eidi, Maryam. "Effects of histamine and cholinergic systems on memory retention of passive avoidance learning in rats." European journal of pharmacology (2003)
de Leon, Jose. "A meta-analysis of worldwide studies demonstrates an association between schizophrenia and tobacco smoking behaviors." Schizophrenia research (2005)
de Leon, Jose. "A meta-analysis of worldwide studies demonstrates an association between schizophrenia and tobacco smoking behaviors." Schizophrenia research (2005)
Last edited: