Westside PUFAs
Member
- Joined
- Feb 4, 2015
- Messages
- 1,972
Follow along with the video below to see how to install our site as a web app on your home screen.
Note: This feature may not be available in some browsers.
Click Here if you want to upgrade your account
If you were able to post but cannot do so now, send an email to admin at raypeatforum dot com and include your username and we will fix that right up for you.
WTF IS THAT? DON'T CALL THAT OLIVE OIL HAVE SOME RESPECT
yes i understand, but honestly would the effect be different with expensive olive oil?
 (maybe)
(maybe)That cup of oil he drank is not coating his RBCs to make them sticky...
That cup of oil he drank is not coating his RBCs to make them sticky...
x2How does this apply to (almost) completely saturated fats like coconut?
Intravascular Aggregation and Adhesiveness of the Blood Elements Associated with Alimentary Lipemia and Injections of Large Molecular Substances | Circulationx2
I would love to see the same experiment repeated with coconut oil.
It was found that the hamsters usually developed a greater alimentary lipemia if they had been on a high fat diet for a period of several days. Most of our animals had been on such a diet for one to three weeks prior to observation and frequently this was supplemented by a daily feeding of cream for 2 to 4 days prior to visualization of their pouches. We have, however, observed a significant lipemia followed by the changes now to be described following a single fat meal without prior large fat feedings.
On the day of visualization the pouch was exposed three to six hours after the fat meal. No change was observed in the circulation during the period of increasing visible lipemia. When the chylomicron count began to fall, usually four to seven hours after the fat meal, changes in the suspension stability of the red blood cells began to develop (fig. 1). First the red blood cells appeared to be slightly adhesive to one another, and here and there a red blood cell stuck momentarily to the wall of a blood vessel or to a white blood cell which was adherent to a vessel wall. The tendency to rouleau formation became more pronounced, the size of these formations increased greatly, and the cells showed a definite tendency to remain together under circumstances which normally would have separated them. Simultaneously the speed of the circulation decreased. This tendency toward aggregation gradually became much greater, and in capillaries and venules red blood cells began to aggregate in irregular small clusters of 4 to 12 or more cells. In many vessels the flow of blood became extremely slow, and frequently the flow stopped completely in some vessels. These changes became first evident and remained most pronounced in the venules.
When the changes just described became pronounced the aggregates of red blood cells assumed an amorphous, homogeneous appearance, and the outlines of the individual cells could no longer be distinguished clearly. Frequently the red blood cells had the appearance of being covered by a surface film. In those vessels in which the rate of flow was greatly reduced, particularly in the venules and smaller veins, the blood flowed in great "chunks" (figs. 3B and C, and 4A and B). When adherent cells separated, one frequently saw them stretched out of shape, and on a few occasions thin viscous strands could be seen attaching them together. At this stage distorted red blood cells were frequently seen, and sometimes clumps of platelets and platelets adhering to red blood cells were observed.
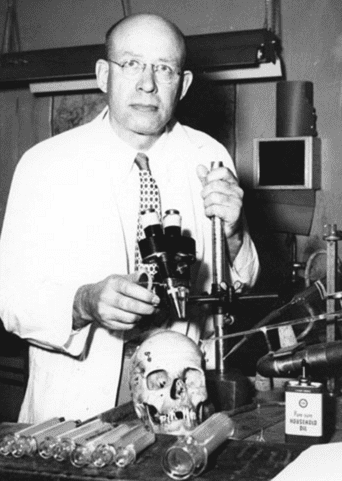
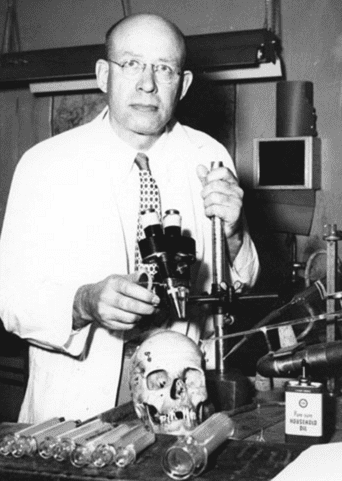
Dr. Knisely did some pioneering research in this. Gotta love his pic:
Sludged Blood. - PubMed - NCBI
IN ABOUT 600 UNANESTHETIZED HUMAN PATIENTS DIAGNOSED BY PRACTICING PHYSICIANS AS HAVING A WIDE VARIETY OF PATHOLOGIC CONDITIONS AND DISEASES, WE HAVE SEEN THE BLOOD CELLS AGGLUTINATED INTO MASSES; THIS CHANGED THE BLOOD FROM ITS NORMAL, RELATIVELY FLUID STATE, TO A CIRCULATING SLUDGE.
Fatty acids, fibrinogen and blood flow: A general mechanism for hyperfibrinogenemia and its pathologic consequences
Plasma fibrinogen is elevated in various stressful states and conditions in which active mobilization of free fatty acids (FFA) occurs. Reduction of plasma FFA by an assortment of hypolipidemic drugs is consistently followed by a decrease in the accompanying hyperfibrinogenemia.
A direct link between FFA and fibrinogen has been demonstrated in animals, and in experiments employing incubated liver slices. Based on these clinical and experimental observations, we postulate that hepatic fibrinogen synthesis is stimulated by FFA. Since fibrinogen is a major determinant of whole blood viscosity, erythrocyte aggregation, and sludging of red cells in terminal and pre-terminal blood vessels, we propose that microcirculatory blood flow may be impaired in the presence of chronically elevated plasma FFA levels. Consequently, hypolipidemic drugs may be effective in prevention of circulatory complications associated with FFA-induced hyperfibrinogenemia.
Fairly, there's probably something intermediate going on. The idea that drinking oil makes that very oil get into your blood in a form that preferentially sticks to cells is whacky. They could be bumping around TGs or big lipoproteins, or those lipoproteins and other TGs could be recruiting monocytic intercellular adhesion molecules. But to simply that the fat it coating the cells themselves and making them sticky is like saying when you eat meat the meat protein goes into your blood and adds to your muscle cells.Are you sure about that?
Fairly, there's probably something intermediate going on. The idea that drinking oil makes that very oil get into your blood in a form that preferentially sticks to cells is whacky. They could be bumping around TGs or big lipoproteins, or those lipoproteins and other TGs could be recruiting monocytic intercellular adhesion molecules. But to simply that the fat it coating the cells themselves and making them sticky is like saying when you eat meat the meat protein goes into your blood and adds to your muscle cells.