Obi-wan
Member
- Joined
- Mar 16, 2017
- Messages
- 1,120
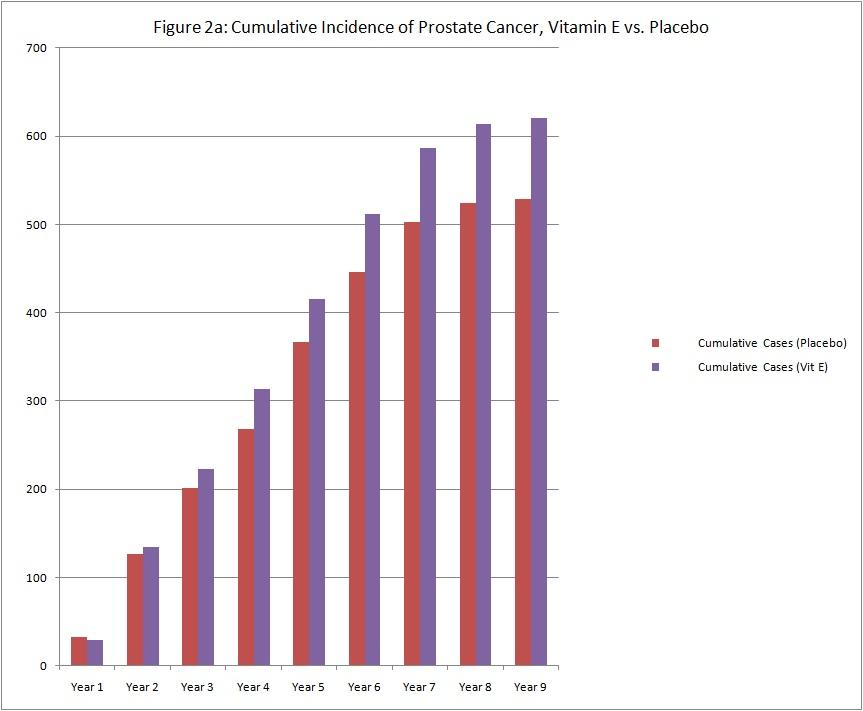
Vitamin E supplementation has not been shown to have significant benefit for people who are healthy, and appears to be harmful.[27][28] It does not improve blood sugar control in an unselected group of people with diabetes mellitus[29] or decrease the risk of stroke.[30] Daily supplementation of vitamin E does not decrease the risk of prostate cancer, and may increase it. -Wikipedia
Sources[edit]
mg/(100 g)
[note 1] Some foods with vitamin E content[3][1][48]
low high
150 Wheat germ oil
95 Almond oil
44 Canola/rapeseed oil
41 Sunflower oil
34 Safflower oil
26 Almonds
19 Wheat germ
15 Hazelnuts
14 Olive oil
8.33 Peanut
1.5 3.4 High-value green, leafy vegetables: spinach, turnip, beet greens, collard greens, and dandelion greens[note 2]
2.32 Butter
2 Avocados
1.8 Cocoa butter
1.4 Sesame oil
1.1 1.5 Asparagus[note 3]
1.5 Kiwifruit (green)
0.90 Cashew nuts
0.78 1.5 Broccoli[note 4]
0.8 1 Pumpkin[note 5]
0.26 0.94 Sweet potato[note 6]
0.9 Mangoes
0.7 Walnuts
0.54 0.56 Tomatoes[note 7]
0.13 0.22 Low-value green, leafy vegetables: lettuce[note 8]
As you can see most are PUFA's
Look at wheat germ oil:
Component g/100g
Linoleic acid (omega-6) 55
Palmitic acid 16
Oleic acid 14
Linolenic acid (omega-3) 7
Very high in Linoleic Acid! As we know from @Travis and Ray, Linoleic acid leads a pathway to proliferation!
I will stay away from Vitamin E and just consume coconut oil which has NO Linoleic or Linolenic acid.
Per Ray- Coconut oil is unusually rich in short and medium chain fatty acids. Shorter chain length allows fatty acids to be metabolized without the use of the carnitine transport system. Mildronate, which I discussed in an article on adaptogens, protects cells against stress partly by opposing the action of carnitine, and comparative studies showed that added carnitine had the opposite effect, promoting the oxidation of unsaturated fats during stress, and increasing oxidative damage to cells. I suspect that a degree of saturation of the oxidative apparatus by short-chain fatty acids has a similar effect--that is, that these very soluble and mobile short-chain saturated fats have priority for oxidation, because they don't require carnitine transport into the mitochondrion, and that this will tend to inhibit oxidation of the unstable, peroxidizable unsaturated fatty acids.
Fatty acid content of coconut oil
Type of fatty acid pct
Caprylic saturated C8
7%
Decanoic saturated C10
8%
Lauric saturated C12
48%
Myristic saturated C14
16%
Palmitic saturated C16
9.5%
Oleic monounsaturated C18:1
6.5%
Other
5%
Per Ray-It is well established that dietary coconut oil reduces our need for vitamin E
Sources[edit]
mg/(100 g)
[note 1] Some foods with vitamin E content[3][1][48]
low high
150 Wheat germ oil
95 Almond oil
44 Canola/rapeseed oil
41 Sunflower oil
34 Safflower oil
26 Almonds
19 Wheat germ
15 Hazelnuts
14 Olive oil
8.33 Peanut
1.5 3.4 High-value green, leafy vegetables: spinach, turnip, beet greens, collard greens, and dandelion greens[note 2]
2.32 Butter
2 Avocados
1.8 Cocoa butter
1.4 Sesame oil
1.1 1.5 Asparagus[note 3]
1.5 Kiwifruit (green)
0.90 Cashew nuts
0.78 1.5 Broccoli[note 4]
0.8 1 Pumpkin[note 5]
0.26 0.94 Sweet potato[note 6]
0.9 Mangoes
0.7 Walnuts
0.54 0.56 Tomatoes[note 7]
0.13 0.22 Low-value green, leafy vegetables: lettuce[note 8]
As you can see most are PUFA's
Look at wheat germ oil:
Component g/100g
Linoleic acid (omega-6) 55
Palmitic acid 16
Oleic acid 14
Linolenic acid (omega-3) 7
Very high in Linoleic Acid! As we know from @Travis and Ray, Linoleic acid leads a pathway to proliferation!
I will stay away from Vitamin E and just consume coconut oil which has NO Linoleic or Linolenic acid.
Per Ray- Coconut oil is unusually rich in short and medium chain fatty acids. Shorter chain length allows fatty acids to be metabolized without the use of the carnitine transport system. Mildronate, which I discussed in an article on adaptogens, protects cells against stress partly by opposing the action of carnitine, and comparative studies showed that added carnitine had the opposite effect, promoting the oxidation of unsaturated fats during stress, and increasing oxidative damage to cells. I suspect that a degree of saturation of the oxidative apparatus by short-chain fatty acids has a similar effect--that is, that these very soluble and mobile short-chain saturated fats have priority for oxidation, because they don't require carnitine transport into the mitochondrion, and that this will tend to inhibit oxidation of the unstable, peroxidizable unsaturated fatty acids.
Fatty acid content of coconut oil
Type of fatty acid pct
Caprylic saturated C8
7%
Decanoic saturated C10
8%
Lauric saturated C12
48%
Myristic saturated C14
16%
Palmitic saturated C16
9.5%
Oleic monounsaturated C18:1
6.5%
Other
5%
Per Ray-It is well established that dietary coconut oil reduces our need for vitamin E
Last edited: