Ray peat has spoken about the negatives of acetylcholine relating to stress and learning
Acetylcholine is an excitotoxic neurotransmitter
Acetylcholine likely raises serotonin in the brain (preferentially inhibits MAO-A in the brain)
https://pubmed.ncbi.nlm.nih.gov/19025057/
AChE inhibitors raise acetylcholine levels -
finding things that raise acetylcholine is easy. AChE inhibition is common, you get this effect from many supplements because plants try to raise acetylcholine in pests to avoid getting eaten. which is why they're used as pesticides by humans too.
 sites.google.com
sites.google.com
ray peat article:
another study:
A simplified way of looking at this could be:
too little ACH = you get under-cognition + brainfog,
too much ACH = you get irritability + overthinking mind + depression/learned helplessness (e.g the state some people get by eating a lot of eggs high in choline) and maybe reduced learning performance too because of that.
looking around , specifically targetting acetylcholine in the HIPPOCAMPUS is especially connected to depression / mood
some things i've found so far to lower acetylcholine:
scopolamine
(but not very accessable & unsure on toxicity in low doses) (also very expensive transdermally - a patch takes >3 hours to hit effects levels for 50% of people, 8 hours to peak, stays elevated by 22 hrs, probably for 3 days https://www.researchgate.net/public...ity_in_combined_oral_and_transdermal_delivery)
https://jamanetwork.com/journals/jamapsychiatry/fullarticle/209881
88% performance vs 82% performance on the cognition test , so gave a slight reduction in cognition . but overall well tolerated on that dose.
is the substance safe or toxic? plant is toxic , and high dose is a hallucinogen 60mg is used to induce memory impairment and 1mg also (swings too much the other way)

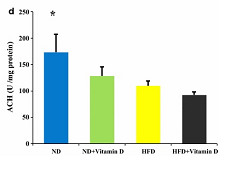
vitamin D ~5000IU for 5 weeks slightly reduces acetylcholine in the hippocampus,
and has a bigger reducing effect in the hypothalamus (similar effect in the hypothalamus with a high fat diet?)
Reduced acetylcholine synthesis in hippocampus and hypothalamus of rats in the current study after vitamin D supplementation was also approved in previous reports; vitamin D has been introduced as an important factor modifying the synthesis of several neuro-mediators like acetylcholine via increased gene expression of the enzyme choline acetyl-transferase (CAT)

things that might have potential to look more at:
- iodine? (probably not in regular doses)
- tyrosine? (but impairs mitochondrial metoblism?)
- low dose bendryl? (but also reduces brain histamine more potently)
- cyproheptadine? (but bunch of other interactions also)
Please post more ways to decrease acetylcholine in the brain
Acetylcholine is an excitotoxic neurotransmitter
antagonism of either nicotinic or muscarinic ACh receptors can have antidepressant effects in humans and decrease stress-relevant behaviors in rodents
Acetylcholine likely raises serotonin in the brain (preferentially inhibits MAO-A in the brain)
https://pubmed.ncbi.nlm.nih.gov/19025057/
AChE inhibitors raise acetylcholine levels -
finding things that raise acetylcholine is easy. AChE inhibition is common, you get this effect from many supplements because plants try to raise acetylcholine in pests to avoid getting eaten. which is why they're used as pesticides by humans too.
Anne Wright - Cholinesterase Inhibitors
Overview Cholinesterase inhibitors (CIs) are neurotoxins which inhibit the action of cholinesterase enzymes. The body uses cholinesterase to break down the neurotransmitter acetylcholine. Inhibition of cholinesterase interferes with the propogation of signals from the brain and central nervous
ray peat article:
Brain trauma consistently leads to decreased activity of this enzyme (Östberg, et al., 2011; Donat, et al., 2007), causing the acetylcholine produced in the brain to accumulate, with many interesting consequences. In 1997, a group (Pike, et al.) created brain injuries in rats to test the idea that a cholinesterase inhibitor would improve their recovery and ability to move through a maze. They found instead that it reduced the cognitive ability of both the injured and normal rats
A series of experiments that started at the University of California in 1960 found that rats that lived in larger spaces with various things to explore were better at learning and solving problems than rats that were raised in the standard little laboratory cages (Krech, et al., 1960). Studying their brains, they found that the enzyme cholinesterase, which destroys the neurotransmitter, acetylcholine, was increased. They later found that the offspring of these rats were better learners than their parents, and their brains contained more cholinesterase.
Their brains were also larger, with a considerable thickening of the cortex, which is considered to be the part mainly responsible for complex behavior, learning and intelligence.
Because cholinergic nerves have been opposed to the sympathetic, adrenergic, nerves, there has been a tendency to neglect their nerve exciting roles, when looking at causes of excitotoxicity, or the stress-induced loss of brain cells. Excessive cholinergic stimulation, however, can contribute to excitotoxic cell death, for example when it's combined with high cortisol and/or hypoglycemia.
In 1976 there was an experiment (Rosellini, et al.) that made an important link between the enrichment experiments and the learned helplessness experiments. The control animals in the enrichment experiments were singly housed, while the others shared a larger enclosure. In the later experiment, it was found that the rats "who were reared in isolation died suddenly when placed in a stressful swimming situation," while the group-housed animals were resistant, effective swimmers. Enrichment and deprivation have very clear biological meaning, and one is the negation of the other.
The increase of cholinesterase, the enzyme that destroys acetylcholine, during enrichment, serves to inactivate cholinergic processes. If deprivation does its harm by increasing the activity of the cholinergic system, we should expect that a cholinergic drug might substitute for inescapable stress, as a cause of learned helplessness, and that an anticholinergic drug could cure learned helplessness. Those tests have been done: "Treatment with the anticholinesterase, physostigmine, successfully mimicked the effects of inescapable shock." "The centrally acting anticholinergic scopolamine hydrobromide antagonized the effects of physostigmine, and when administered prior to escape testing antagonized the disruptive effects of previously administered inescapable shock."
another study:
A crucial finding is the loss of acetylcholinesterase activity with mitochondrial dysfunction globally in the brain of hypercholesterolemic mice
A simplified way of looking at this could be:
too little ACH = you get under-cognition + brainfog,
too much ACH = you get irritability + overthinking mind + depression/learned helplessness (e.g the state some people get by eating a lot of eggs high in choline) and maybe reduced learning performance too because of that.
looking around , specifically targetting acetylcholine in the HIPPOCAMPUS is especially connected to depression / mood
brain ACh levels increase in response to stressful challenges, whereas systemically blocking acetylcholinesterase (AChE, the primary ACh degradative enzyme) elicits depression-like symptoms in human subjects, and selectively blocking AChE in the hippocampus increases relevant behaviors in rodents
These studies suggest that ACh signaling results in maladaptive behavioral responses to stress if the balance of signaling is shifted toward increased hippocampal engagement.
some things i've found so far to lower acetylcholine:
scopolamine
(but not very accessable & unsure on toxicity in low doses) (also very expensive transdermally - a patch takes >3 hours to hit effects levels for 50% of people, 8 hours to peak, stays elevated by 22 hrs, probably for 3 days https://www.researchgate.net/public...ity_in_combined_oral_and_transdermal_delivery)
https://jamanetwork.com/journals/jamapsychiatry/fullarticle/209881
in a human trial , scopolamine (which reduces acetylcholine through antagonizing muscarinic receptors) reduces depressionAcetylcholine (ACh) levels are elevated in actively depressed subjects
88% performance vs 82% performance on the cognition test , so gave a slight reduction in cognition . but overall well tolerated on that dose.
orally - mice study tiny dose orally works and higher dose reverse effects? 0.1mg humanScopolamine produced rapid and robust antidepressant and antianxiety effects in patients with unipolar and bipolar depression.
Significant clinical responses were observed in the evaluation after the first scopolamine administration, 3 to 4 days after the first treatment
scopolamine hydrobromide (4 μg/kg intravenously)
is the substance safe or toxic? plant is toxic , and high dose is a hallucinogen 60mg is used to induce memory impairment and 1mg also (swings too much the other way)
vitamin D ~5000IU for 5 weeks slightly reduces acetylcholine in the hippocampus,
and has a bigger reducing effect in the hypothalamus (similar effect in the hypothalamus with a high fat diet?)
Reduced acetylcholine synthesis in hippocampus and hypothalamus of rats in the current study after vitamin D supplementation was also approved in previous reports; vitamin D has been introduced as an important factor modifying the synthesis of several neuro-mediators like acetylcholine via increased gene expression of the enzyme choline acetyl-transferase (CAT)

things that might have potential to look more at:
- iodine? (probably not in regular doses)
- tyrosine? (but impairs mitochondrial metoblism?)
- low dose bendryl? (but also reduces brain histamine more potently)
- cyproheptadine? (but bunch of other interactions also)
Please post more ways to decrease acetylcholine in the brain
Attachments
Last edited: