Navigation
Install the app
How to install the app on iOS
Follow along with the video below to see how to install our site as a web app on your home screen.
Note: This feature may not be available in some browsers.
More options
-
By using this site you agree to the terms, rules, and privacy policy.
-
Charlie's Restoration Giveaway #2 (Entire Home EMF Mitigation & Protection Along With Personal Protection) - Click Here To Enter
-
Dear Carnivore Dieters, A Muscle Meat Only Diet is Extremely Healing Because it is a Low "vitamin A" Diet. This is Why it Works so Well...
Rest the rest of this post by clicking here
-
The Forum is transitioning to a subscription-based membership model - Click Here To Read
Click Here if you want to upgrade your account
If you were able to post but cannot do so now, send an email to admin at raypeatforum dot com and include your username and we will fix that right up for you.
You are using an out of date browser. It may not display this or other websites correctly.
You should upgrade or use an alternative browser.
You should upgrade or use an alternative browser.
Help in finding Covid studies on respirators with only oxygen vs carbogen (5% CO2).
- Thread starter Yann
- Start date
Hi Yann, I had the same exact thought, when, in 2020, I first read about oxygen given to Covid patients and intubation in hospital settings. Are they using pure oxygen and thereby killing patients?? Does anybody know what is used in hospitals? Are there any CDC guidelines?I remember Ray saying that hospitals using carbogen instead of oxygen had higher recevery rates but I can't find any studies on that. I think he was refering to hospitals in Europe. Has anyone found studies on that? Thanks!
P
Peatness
Guest
The May 2020 newsletter - This Novel Flu Season might have this information
Perry Staltic
Member
- Joined
- Dec 14, 2020
- Messages
- 8,186
Hi Yann, I had the same exact thought, when, in 2020, I first read about oxygen given to Covid patients and intubation in hospital settings. Are they using pure oxygen and thereby killing patients?? Does anybody know what is used in hospitals? Are there any CDC guidelines?
They crank up FiO2 until they can't go any farther, i.e., 100% Huge damage to lungs via ROS.
Yes, they are using pure oxygen. The carbogen practice is never used, IIRC. But even worse than oxygen are ventilators that push oxygen into the lungs with force. Ray talked about this last year and sent me this link: Is protocol-driven COVID-19 respiratory therapy doing more harm than good?Hi Yann, I had the same exact thought, when, in 2020, I first read about oxygen given to Covid patients and intubation in hospital settings. Are they using pure oxygen and thereby killing patients?? Does anybody know what is used in hospitals? Are there any CDC guidelines?
Experience shows that mortality in ICUs could be completely eliminated if they would only change the protocols. Imagine how many "covid deaths" must then be due solely to innapropriate treatment with oxygen.
"Anecdotal evidence has increasingly demonstrated that this proposed physiological approach is associated with much lower mortality rates among COVID-19 patients, he said.
While not willing to name the hospitals at this time, he said that one center in Europe has had a 0% mortality rate among COVID-19 patients in the ICU when using this approach, compared with a 60% mortality rate at a nearby hospital using a protocol-driven approach."
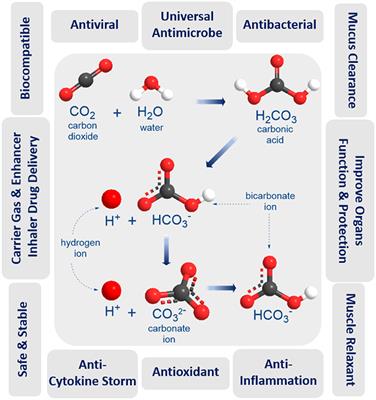
Humidified Warmed CO2 Treatment Therapy Strategies Can Save Lives With Mitigation and Suppression of SARS-CoV-2 Infection: An Evidence Review
The coronavirus disease (COVID-19) outbreak has presented enormous challenges for healthcare, societal, and economic systems worldwide. There is an urgent global need for a universal vaccine to cover all SARS-CoV-2 mutant strains to stop the current COVID-19 pandemic and the threat of an...
Very interesting! Dr. Mercola recommends humidifying saline solution with small amounts of hydrogen peroxide. He recommends to use food-grade hydrogen peroxide and dilute it down to 0.1% using the saline solution.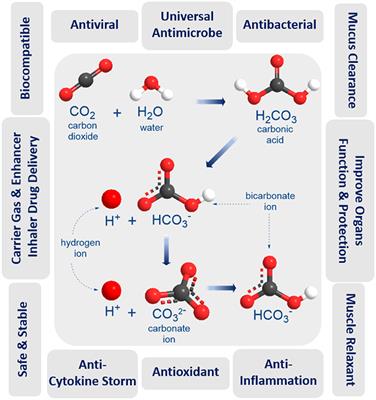
Humidified Warmed CO2 Treatment Therapy Strategies Can Save Lives With Mitigation and Suppression of SARS-CoV-2 Infection: An Evidence Review
The coronavirus disease (COVID-19) outbreak has presented enormous challenges for healthcare, societal, and economic systems worldwide. There is an urgent global need for a universal vaccine to cover all SARS-CoV-2 mutant strains to stop the current COVID-19 pandemic and the threat of an...www.frontiersin.org
md_a
Member
- Joined
- Aug 31, 2015
- Messages
- 468
Lewis S Coleman
American Institute of Stress
The therapeutic benefits of dioxide were understood 100 years ago. Anyone interested in this subject might be interested in my review of this history called "Four Forgotten Giants of Anesthesia History"
Four Forgotten Giants of Anesthesia History
....................
An idea: Could we prevent the development of ARDS in COVID-19 patients by administering carbon dioxide and oxygen? (Calling for collective thinking.)
Andras Sikter
Budapest, Szent Rókus Kórház
It has already applied the principles of 'permissive hypercapnia' during mechanical ventilation in several clinics at ARDS of COVID-19 patients, which is likely to save lives. Nevertheless, treating ARDS with mechanical ventilation is not a 21st-century solution[2].
I had stated that hypocapnia could cause vicious circles and death at critically ill patients[1].
Several vicious circles have also been identified in ARDS, and hypocapnia may also play a role in them, for example, enhances pulmonary hypertension[3] and decreases surfactant formation[4].
Does the question arise, whether the vicious circles can be stopped even before ARDS develops?
Surprisingly few works of literature are known to use a mixture of carbon dioxide and oxygen therapeutically at any disorders. Administration of 5% carboxygene in animal experiments reversed the process of surfactant depletion.
Laffey effect of hypocapnia on surfactant.pdf
Repesse-2017-Right-heart-function-during-acute-r.pdf
Schmidt-2017-Will-all-ards-patients-be-receiving (1).pdf
…………
@Giannoni et al. successfully influenced pCO2 levels during Cheyne-Stokes respiration: "dynamic CO2 administration, delivered at an appropriate time during periodic breathing, can almost eliminate oscillations in end-tidal CO2 and ventilation.” During the procedure, the average pCO2 level increased, and there was a moderate increase in respiratory volume. The introduction of the method in the early stage of ARDS may be beneficial, as the increase in metabolism in hyperventilation is mostly due to the decreased pCO2 levels.
@Khambatta HJ and Sullivan SF (1974) mechanically hyperventilated dogs for several hours. Energy expenditure increased significantly, which could not originate from the 'work of breathing' because the hyperventilation was passive during the study. In summary, it is in principle possible to reduce the increased metabolism caused by hyperventilation.
https://journals.physiology.org/doi/pdf/10.1152/jappl.1974.37.5.665
Giannoni-2010-Real-time-dynamic-carbon-dioxide-ad (2).pdf
………..
Thank you for sharing this information. Carbon dioxide supplementation therapy is not a medicament. It is pathophysiology.
Dead space ventilation promotes alveolar hypocapnia reducing surfactant secretion by altering mitochondrial function | Thorax
............
Andras Sikter
Budapest, Szent Rókus Kórház
The permissive hypercapnia is already widely accepted. (See Hamilton Medical's protocol (attached) This is only another method. Combined with mechanical ventilation is a safe mode to try it. I have discussed it with @john Laffey (who is one of the inventors of permissive hypercapnia). He has found the idea to be inventive and distinct. He maybe applies it.
hamilton-knowledgebase-PERMISSIVE HYPERCAPNIA- COVID-1
9-ARDS.pdf
………..
Andras Sikter
Budapest, Szent Rókus Kórház
Thank you for your answer. I have been looking for the effects of CO2 on biological systems. I hope that ARDS could be prevented at an early stage. It can be reversing the vicious circles by administering carbogen. I know that CO2 administration can cause a massive increase in respiratory volume, which is undesirable. I hope that the concomitant administration of bicarbonate will prevent a significant volume increase in breathing. It would compensate for the hypercapnia. It is probable that the protective effects of permissive hypercapnia depend on pCO2 levels and not pH, because intracellular pH correlates with pCO2 during acute hypercapnia. I should like to study the relevant literature. And why is all this? COVID-19 comes to poor African and Asian countries who have no ventilator machines ... You should help developing countries with working out new, cheaper methods.
………….
The method of permissive hypercapnia is now widely accepted in treating ARDS during mechanical ventilation as opposed to the traditional one, although there is still no agreement on the standards. Several doctors consider the possibility of a decrease in pH and an increase in pCO2 to be almost limitless. @Josh Farkas would draw the boundaries for both 'permissive pH' and 'permissive pCO2' []. According to him, one of the studies about permissive hypercapnia performed one of the best results because the Na-bicarbonate infusion was allowed [].
PulmCrit- Extracorporeal CO2 removal: Putting the cart ahead of the horse?
2000-Ventilation-with-lower-tidal-volume.pdf
……….
Andras Sikter
Budapest, Szent Rókus Kórház
Thank you for your valuable answer. You mentioned 'increased sympathetic activity' plays a significant role in COVID-ARDS.
It can be presented that hypocapnia and the vicious circle maintained by hypocapnia play a critical role in the perpetually increasing sympathetic activity. (See my article).
I accept that ‘permissive hypercapnia’ has a colossal regulator to cool down this increased sympathetic activity and that it can be sustained for days without tissue damage. It is an (almost) physiological process. I would like to point out that you should attempt to interrupt the vicious circles of sympathetic activity maintained by hyperventilation/ hypocapnia in the 'pre-ARDS' phase by co-administration of carboxygen and Na-bicarbonate - without mechanical ventilation. On the one hand, there is no ventilator machine for everyone and everywhere (think about Africa). On the other hand, mechanical ventilation is not physiological either, and it would be better to prevent trouble, not to cure it when it is already advanced.
(PDF) Hypocapnia and mental stress can trigger vicious circles in critically ill patients due to energy imbalance: a hypothesis presented through cardiogenic pulmonary oedema
……………
Can hypocapnia trigger ARDS and kill coronavirus diseased patients?
May 2020
DOI:10.13140/RG.2.2.11566.25929
(PDF) Can hypocapnia trigger ARDS and kill coronavirus diseased patients?
.............
Andras Sikter
Budapest, Szent Rókus Kórház
Several works of literature demonstrate that hypocapnia (and not metabolic alkalosis!) plays a significant role in the inhibition of surfactant formation.
https://www.atsjournals.org/doi/full/10.1164/rccm.200408-998OC
Today, it also seems to be proven that this is caused by an increase in mitochondrial Ca2+ levels, which means ATP-energy insufficiency.
Dead space ventilation promotes alveolar hypocapnia reducing surfactant secretion by altering mitochondrial function | Thorax
We do not know how reversible this process is. Ventilator-induced ‘permissive hypercapnia’ already works well, but it’s a little too late for many.
https://www.nejm.org/doi/full/10.1056/nejmra012457
THEREFORE, the lack of surfactant and the development of ARDS should be prevented by raising pCO2 level in anyhow (not with respiratory machinery!). Maybe it's not that hard? At an early stage, perhaps the administration of a small dose of iv. Na-bicarbonate would be sufficient (monitored), taking care not to develop metabolic alkalosis, as well. Therefore, it may still need to be co-administered with carbogen and/or intracellular pCO2-boosting medicine (acetazolamide?).
Role of Hypocapnia in the Alveolar Surfactant Increase Induced by Free Fatty Acid Intravenous Infusion in the Rabbit
IDH3 mediates apoptosis of alveolar epithelial cells type 2 due to mitochondrial Ca2+ uptake during hypocapnia - Cell Death & Disease
.............
Andras Sikter
Budapest, Szent Rókus Kórház
Research Features British magazine presents one of my articles and highlights the role of acute hypocapnia in diseases. Hypocapnia can trigger vicious circles which may lead to a fatal outcome if the body has no energy reserves and is unable to meet the challenge posed by hypocapnia.
The challenge of meeting energy demands during acute hypocapnia
…………………………….
Conclusions
Carbon dioxide is much more than simply metabolic waste: it is a potent biological agent with a range of actions upon cells, and with immune modulating effects at both respiratory and systemic level.
Although preclinical studies indicate a beneficial effect of hypercapnic acidosis in terms of a decrease in ventilator[1]induced lung injury (VILI), there are also adverse effects as evidenced by clinical studies in which an increase in mortality among ARDS patients has been observed. Further randomized clinical studies are needed to establish the true impact of hypercapnia in these patients.
The use of ECCO2R could be important as an adjuvant strategy in the management of patients with ARDS in the absence of severe hypoxemia, allowing ultraprotective ventilation, reducing the risk of VILI, and controlling the PaCO2 levels.
We consider it important to define ideal PaCO2 levels in order to balance their favorable and unfavorable biological effects.
Importance of carbon dioxide in the critical patient: Implications at the cellular and clinical levels | Medicina Intensiva
.....................
An idea: Could we prevent the development of ARDS in COVID-19...
American Institute of Stress
The therapeutic benefits of dioxide were understood 100 years ago. Anyone interested in this subject might be interested in my review of this history called "Four Forgotten Giants of Anesthesia History"
Abstract
The anesthesiology profession may one day serve as a cautionary tale of how power, politics and privilege can perturb science and progress. Previous anesthesia practitioners possessed a superior understanding of physiology and pharmacology, but overenthusiastic CO2 supplementation with inadequate monitors and machines caused asphyxiation disasters that were improperly attributed to CO2 toxicity. Dr. Ralph Waters founded the anesthesiology profession on the basis of a practical new anesthetic technique that introduced elective intubation and hyperventilation to eliminate CO2 toxicity, but mechanical hyperventilation dangerously depletes CO2 tissue reserves and exaggerates morbidity and mortality. The benefits of CO2 supplementations were forgotten, and consequent CO2 confusion has derailed research, discouraged opioid treatment, damaged patient safety, and disrupted professional progress. Anesthesiologists can no longer claim to provide superior service, and hospital administrators are replacing them with nurses. Professional membership is in decline, and professional survival is in question. Modern machines have eliminated asphyxiation, and modern monitoring enables safe and beneficial hypercarbia that complements opioid treatment and minimizes surgical morbidity and mortality. CO2 reform promises revolutionary advance but faces formidable opposition.Four Forgotten Giants of Anesthesia History
....................
An idea: Could we prevent the development of ARDS in COVID-19 patients by administering carbon dioxide and oxygen? (Calling for collective thinking.)
Andras Sikter
Budapest, Szent Rókus Kórház
It has already applied the principles of 'permissive hypercapnia' during mechanical ventilation in several clinics at ARDS of COVID-19 patients, which is likely to save lives. Nevertheless, treating ARDS with mechanical ventilation is not a 21st-century solution[2].
I had stated that hypocapnia could cause vicious circles and death at critically ill patients[1].
Several vicious circles have also been identified in ARDS, and hypocapnia may also play a role in them, for example, enhances pulmonary hypertension[3] and decreases surfactant formation[4].
Does the question arise, whether the vicious circles can be stopped even before ARDS develops?
Surprisingly few works of literature are known to use a mixture of carbon dioxide and oxygen therapeutically at any disorders. Administration of 5% carboxygene in animal experiments reversed the process of surfactant depletion.
Laffey effect of hypocapnia on surfactant.pdf
Repesse-2017-Right-heart-function-during-acute-r.pdf
Schmidt-2017-Will-all-ards-patients-be-receiving (1).pdf
…………
@Giannoni et al. successfully influenced pCO2 levels during Cheyne-Stokes respiration: "dynamic CO2 administration, delivered at an appropriate time during periodic breathing, can almost eliminate oscillations in end-tidal CO2 and ventilation.” During the procedure, the average pCO2 level increased, and there was a moderate increase in respiratory volume. The introduction of the method in the early stage of ARDS may be beneficial, as the increase in metabolism in hyperventilation is mostly due to the decreased pCO2 levels.
@Khambatta HJ and Sullivan SF (1974) mechanically hyperventilated dogs for several hours. Energy expenditure increased significantly, which could not originate from the 'work of breathing' because the hyperventilation was passive during the study. In summary, it is in principle possible to reduce the increased metabolism caused by hyperventilation.
https://journals.physiology.org/doi/pdf/10.1152/jappl.1974.37.5.665
Giannoni-2010-Real-time-dynamic-carbon-dioxide-ad (2).pdf
………..
Thank you for sharing this information. Carbon dioxide supplementation therapy is not a medicament. It is pathophysiology.
Dead space ventilation promotes alveolar hypocapnia reducing surfactant secretion by altering mitochondrial function | Thorax
............
Andras Sikter
Budapest, Szent Rókus Kórház
The permissive hypercapnia is already widely accepted. (See Hamilton Medical's protocol (attached) This is only another method. Combined with mechanical ventilation is a safe mode to try it. I have discussed it with @john Laffey (who is one of the inventors of permissive hypercapnia). He has found the idea to be inventive and distinct. He maybe applies it.
hamilton-knowledgebase-PERMISSIVE HYPERCAPNIA- COVID-1
9-ARDS.pdf
………..
Andras Sikter
Budapest, Szent Rókus Kórház
Thank you for your answer. I have been looking for the effects of CO2 on biological systems. I hope that ARDS could be prevented at an early stage. It can be reversing the vicious circles by administering carbogen. I know that CO2 administration can cause a massive increase in respiratory volume, which is undesirable. I hope that the concomitant administration of bicarbonate will prevent a significant volume increase in breathing. It would compensate for the hypercapnia. It is probable that the protective effects of permissive hypercapnia depend on pCO2 levels and not pH, because intracellular pH correlates with pCO2 during acute hypercapnia. I should like to study the relevant literature. And why is all this? COVID-19 comes to poor African and Asian countries who have no ventilator machines ... You should help developing countries with working out new, cheaper methods.
………….
The method of permissive hypercapnia is now widely accepted in treating ARDS during mechanical ventilation as opposed to the traditional one, although there is still no agreement on the standards. Several doctors consider the possibility of a decrease in pH and an increase in pCO2 to be almost limitless. @Josh Farkas would draw the boundaries for both 'permissive pH' and 'permissive pCO2' []. According to him, one of the studies about permissive hypercapnia performed one of the best results because the Na-bicarbonate infusion was allowed [].
PulmCrit- Extracorporeal CO2 removal: Putting the cart ahead of the horse?
2000-Ventilation-with-lower-tidal-volume.pdf
……….
Andras Sikter
Budapest, Szent Rókus Kórház
Thank you for your valuable answer. You mentioned 'increased sympathetic activity' plays a significant role in COVID-ARDS.
It can be presented that hypocapnia and the vicious circle maintained by hypocapnia play a critical role in the perpetually increasing sympathetic activity. (See my article).
I accept that ‘permissive hypercapnia’ has a colossal regulator to cool down this increased sympathetic activity and that it can be sustained for days without tissue damage. It is an (almost) physiological process. I would like to point out that you should attempt to interrupt the vicious circles of sympathetic activity maintained by hyperventilation/ hypocapnia in the 'pre-ARDS' phase by co-administration of carboxygen and Na-bicarbonate - without mechanical ventilation. On the one hand, there is no ventilator machine for everyone and everywhere (think about Africa). On the other hand, mechanical ventilation is not physiological either, and it would be better to prevent trouble, not to cure it when it is already advanced.
(PDF) Hypocapnia and mental stress can trigger vicious circles in critically ill patients due to energy imbalance: a hypothesis presented through cardiogenic pulmonary oedema
……………
Can hypocapnia trigger ARDS and kill coronavirus diseased patients?
May 2020
DOI:10.13140/RG.2.2.11566.25929
(PDF) Can hypocapnia trigger ARDS and kill coronavirus diseased patients?
.............
Andras Sikter
Budapest, Szent Rókus Kórház
Several works of literature demonstrate that hypocapnia (and not metabolic alkalosis!) plays a significant role in the inhibition of surfactant formation.
https://www.atsjournals.org/doi/full/10.1164/rccm.200408-998OC
Today, it also seems to be proven that this is caused by an increase in mitochondrial Ca2+ levels, which means ATP-energy insufficiency.
Dead space ventilation promotes alveolar hypocapnia reducing surfactant secretion by altering mitochondrial function | Thorax
We do not know how reversible this process is. Ventilator-induced ‘permissive hypercapnia’ already works well, but it’s a little too late for many.
https://www.nejm.org/doi/full/10.1056/nejmra012457
THEREFORE, the lack of surfactant and the development of ARDS should be prevented by raising pCO2 level in anyhow (not with respiratory machinery!). Maybe it's not that hard? At an early stage, perhaps the administration of a small dose of iv. Na-bicarbonate would be sufficient (monitored), taking care not to develop metabolic alkalosis, as well. Therefore, it may still need to be co-administered with carbogen and/or intracellular pCO2-boosting medicine (acetazolamide?).
Role of Hypocapnia in the Alveolar Surfactant Increase Induced by Free Fatty Acid Intravenous Infusion in the Rabbit
IDH3 mediates apoptosis of alveolar epithelial cells type 2 due to mitochondrial Ca2+ uptake during hypocapnia - Cell Death & Disease
.............
Andras Sikter
Budapest, Szent Rókus Kórház
Research Features British magazine presents one of my articles and highlights the role of acute hypocapnia in diseases. Hypocapnia can trigger vicious circles which may lead to a fatal outcome if the body has no energy reserves and is unable to meet the challenge posed by hypocapnia.
The challenge of meeting energy demands during acute hypocapnia
…………………………….
Conclusions
Carbon dioxide is much more than simply metabolic waste: it is a potent biological agent with a range of actions upon cells, and with immune modulating effects at both respiratory and systemic level.
Although preclinical studies indicate a beneficial effect of hypercapnic acidosis in terms of a decrease in ventilator[1]induced lung injury (VILI), there are also adverse effects as evidenced by clinical studies in which an increase in mortality among ARDS patients has been observed. Further randomized clinical studies are needed to establish the true impact of hypercapnia in these patients.
The use of ECCO2R could be important as an adjuvant strategy in the management of patients with ARDS in the absence of severe hypoxemia, allowing ultraprotective ventilation, reducing the risk of VILI, and controlling the PaCO2 levels.
We consider it important to define ideal PaCO2 levels in order to balance their favorable and unfavorable biological effects.
Importance of carbon dioxide in the critical patient: Implications at the cellular and clinical levels | Medicina Intensiva
.....................
An idea: Could we prevent the development of ARDS in COVID-19...
Attachments
-
2000-Ventilation-with-lower-tidal-volume.pdf179.6 KB · Views: 4
-
Carbon dioxide production and washout during passive hyperventilation alkalosis.pdf964.8 KB · Views: 3
-
Dead space ventilation promotes alveolar hypocapnia reducing surfactant secretion by altering ...pdf6.8 MB · Views: 3
-
Four-Forgotten-Giants-of-Anesthesia-History.pdf442.2 KB · Views: 3
-
Giannoni-2010-Real-time-dynamic-carbon-dioxide-ad2.pdf502.9 KB · Views: 3
-
hamilton-knowledgebase-PERMISSIVEHYPERCAPNIA-COVID-19-ARDS.pdf49.8 KB · Views: 3
-
Henderson CARBON DIOXIDE EDIT in red.doc68.5 KB · Views: 3
-
Henderson CO2 treat Pneumonia archinte_45_1_0.pdf5.4 MB · Views: 3
-
Importance of carbon dioxide in the critical patient.pdf1.1 MB · Views: 7
-
Laffeyeffectofhypocapniaonsurfactant.pdf79.3 KB · Views: 3
Beastmode
Member
- Joined
- Feb 7, 2017
- Messages
- 1,258
When my late grandma was in the hospital, we pushed for carbogen instead of the pure oxygen, via mask, they were giving her.
Unfortunately, it was during COVID so no one could be in the hospital so everything was done over the phone.
Unfortunately, it was during COVID so no one could be in the hospital so everything was done over the phone.
EMF Mitigation - Flush Niacin - Big 5 Minerals
Similar threads
- Replies
- 6
- Views
- 3K
- Replies
- 155
- Views
- 26K
- Replies
- 11
- Views
- 4K
- Replies
- 50
- Views
- 26K
- Replies
- 0
- Views
- 830
- Replies
- 5
- Views
- 1K
- Replies
- 1
- Views
- 2K
- Replies
- 1
- Views
- 5K
- Replies
- 9
- Views
- 4K
- Replies
- 168
- Views
- 14K
- Replies
- 94
- Views
- 25K
- Replies
- 28
- Views
- 5K
- Replies
- 37
- Views
- 6K
