Mito
Member
- Joined
- Dec 10, 2016
- Messages
- 2,554
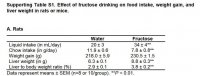
It would be good to know what they fed the rats and mice including exactly how much fructose they ingested.
Abstract
Fructose intake is known to induce obesity, insulin resistance, metabolic syndrome, and nonalcoholic fatty liver disease (NAFLD). We aimed to evaluate the effects of fructose drinking on gut leakiness, endotoxemia, and NAFLD and study the underlying mechanisms in rats, mice, and T84 colon cells. Levels of ileum junctional proteins, oxidative stress markers, and apoptosis‐related proteins in rodents, T84 colonic cells, and human ileums were determined by immunoblotting, immunoprecipitation, and immunofluorescence analyses. Fructose drinking caused microbiome change, leaky gut, and hepatic inflammation/fibrosis with increased levels of nitroxidative stress marker proteins cytochrome P450‐2E1 (CYP2E1), inducible nitric oxide synthase, and nitrated proteins in small intestine and liver of rodents. Fructose drinking significantly elevated plasma bacterial endotoxin levels, likely resulting from decreased levels of intestinal tight junction (TJ) proteins (zonula occludens 1, occludin, claudin‐1, and claudin‐4), adherent junction (AJ) proteins (β‐catenin and E‐cadherin), and desmosome plakoglobin, along with α‐tubulin, in wild‐type rodents, but not in fructose‐exposed Cyp2e1‐null mice. Consistently, decreased intestinal TJ/AJ proteins and increased hepatic inflammation with fibrosis were observed in autopsied obese people compared to lean individuals. Furthermore, histological and biochemical analyses showed markedly elevated hepatic fibrosis marker proteins in fructose‐exposed rats compared to controls. Immunoprecipitation followed by immunoblot analyses revealed that intestinal TJ proteins were nitrated and ubiquitinated, leading to their decreased levels in fructose‐exposed rats.
Conclusion: These results showed that fructose intake causes protein nitration of intestinal TJ and AJ proteins, resulting in increased gut leakiness, endotoxemia, and steatohepatitis with liver fibrosis, at least partly, through a CYP2E1‐dependent manner.
https://aasldpubs.onlinelibrary.wiley.com/doi/abs/10.1002/hep.30652
Abstract
Fructose intake is known to induce obesity, insulin resistance, metabolic syndrome, and nonalcoholic fatty liver disease (NAFLD). We aimed to evaluate the effects of fructose drinking on gut leakiness, endotoxemia, and NAFLD and study the underlying mechanisms in rats, mice, and T84 colon cells. Levels of ileum junctional proteins, oxidative stress markers, and apoptosis‐related proteins in rodents, T84 colonic cells, and human ileums were determined by immunoblotting, immunoprecipitation, and immunofluorescence analyses. Fructose drinking caused microbiome change, leaky gut, and hepatic inflammation/fibrosis with increased levels of nitroxidative stress marker proteins cytochrome P450‐2E1 (CYP2E1), inducible nitric oxide synthase, and nitrated proteins in small intestine and liver of rodents. Fructose drinking significantly elevated plasma bacterial endotoxin levels, likely resulting from decreased levels of intestinal tight junction (TJ) proteins (zonula occludens 1, occludin, claudin‐1, and claudin‐4), adherent junction (AJ) proteins (β‐catenin and E‐cadherin), and desmosome plakoglobin, along with α‐tubulin, in wild‐type rodents, but not in fructose‐exposed Cyp2e1‐null mice. Consistently, decreased intestinal TJ/AJ proteins and increased hepatic inflammation with fibrosis were observed in autopsied obese people compared to lean individuals. Furthermore, histological and biochemical analyses showed markedly elevated hepatic fibrosis marker proteins in fructose‐exposed rats compared to controls. Immunoprecipitation followed by immunoblot analyses revealed that intestinal TJ proteins were nitrated and ubiquitinated, leading to their decreased levels in fructose‐exposed rats.
Conclusion: These results showed that fructose intake causes protein nitration of intestinal TJ and AJ proteins, resulting in increased gut leakiness, endotoxemia, and steatohepatitis with liver fibrosis, at least partly, through a CYP2E1‐dependent manner.
https://aasldpubs.onlinelibrary.wiley.com/doi/abs/10.1002/hep.30652