Koveras
Member
- Joined
- Dec 17, 2015
- Messages
- 720
I am getting the impression that anything which leads to reduced blood flow, including prostaglandin D₂, plays a role. I think cortisol is necessary to explain the hormonal effects, interferon-γ and prostaglandins to explain the immunogenic effects, vitamin D accounting for sun, and other forms of reduced blood flow to explain the rest. If prostaglandin D₂ can be linked to arterial constriction—and it certainly can, as shown below—then it could perhaps be viewed as acting ultimately in this way: the final downstream process. Seeing ischemia and reduced blood flow as the ultimate cause actually makes nearly all popular explanations synergistic, the apparent competition between them perhaps being merely a lack of understanding.
'Prostaglandin D₂ is a powerful antiaggregatory agent and contracts various types of smooth muscle preparations, including isolated canine and bovine pulmonary vessels.' ―Cassin
'Prostaglandin D₂ was originally described by Nugteren and Hazelhof (17) as being biologically inactive. However, in 1975, Hamberg et al. (9) described vasopressor responses to PGD₂ as well as bronchoconstrictor activity in experiments on guinea pigs. Other studies (11, 12) have provided evidence of smooth muscle stimulatory activity of PGD₂ in a variety of species. In 1976, Jones (12) demonstrated pressor activity of PGD₂ in sheep. Additional data have been accumulated to show that PGD₂ increases canine pulmonary vascular resistance (14, 25) and contracts isolated bovine and canine intrapulmonary vessels (8).' ―Cassin
The Cassin experiment had only measured bronchial resistance, but he cites Hamberg and Jones as having shown pressor effects in arteries. The article by Jones—'Cardiovascular actions of prostaglandins D and E in the sheep: evidence for two distinct receptors'— stands out; not only because it includes the phrase 'in the sheep,' but because it apparently has the hard data which demonstrates this.
Hamberg, Mats. "Prostaglandin endoperoxides IV. Effects on smooth muscle." Life sciences (1975)
Cassin, S. "Effects of prostaglandin D2 on perinatal circulation." American Journal of Physiology-Heart and Circulatory Physiology (1981)
Jones, R. L. "Cardiovascular actions of prostaglandins D and E in the sheep: evidence for two distinct receptors." Advances in prostaglandin and thromboxane research (1976).
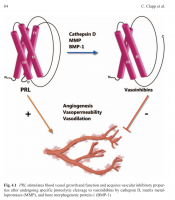
I have an as of yet unpublished theory (Koveras, 2018) that one of the mechanisms prolactin contributes to hair loss is from being cleaved to vasoinhibins.
"Prolactin acquires antiangiogenic properties after undergoing proteolytic cleavage to vasoinhibins, a family of PRL fragments (including 16 kDa PRL) with potent antiangiogenic, vasoconstrictive, and antivasopermeability effects."
I imagine factors which upregulate Cathepsin D, MMPs, and BMP-1 (and thus contribute to this cleavage) will contribute to hair loss.
Clapp, C., Thebault, S., Macotela, Y., Moreno-Carranza, B., Triebel, J., & Martinez de la Escalera, G. (2015). Regulation of blood vessels by prolactin and vasoinhibins. Adv Exp Med Biol, 846, 83-95. doi:10.1007/978-3-319-12114-7_4