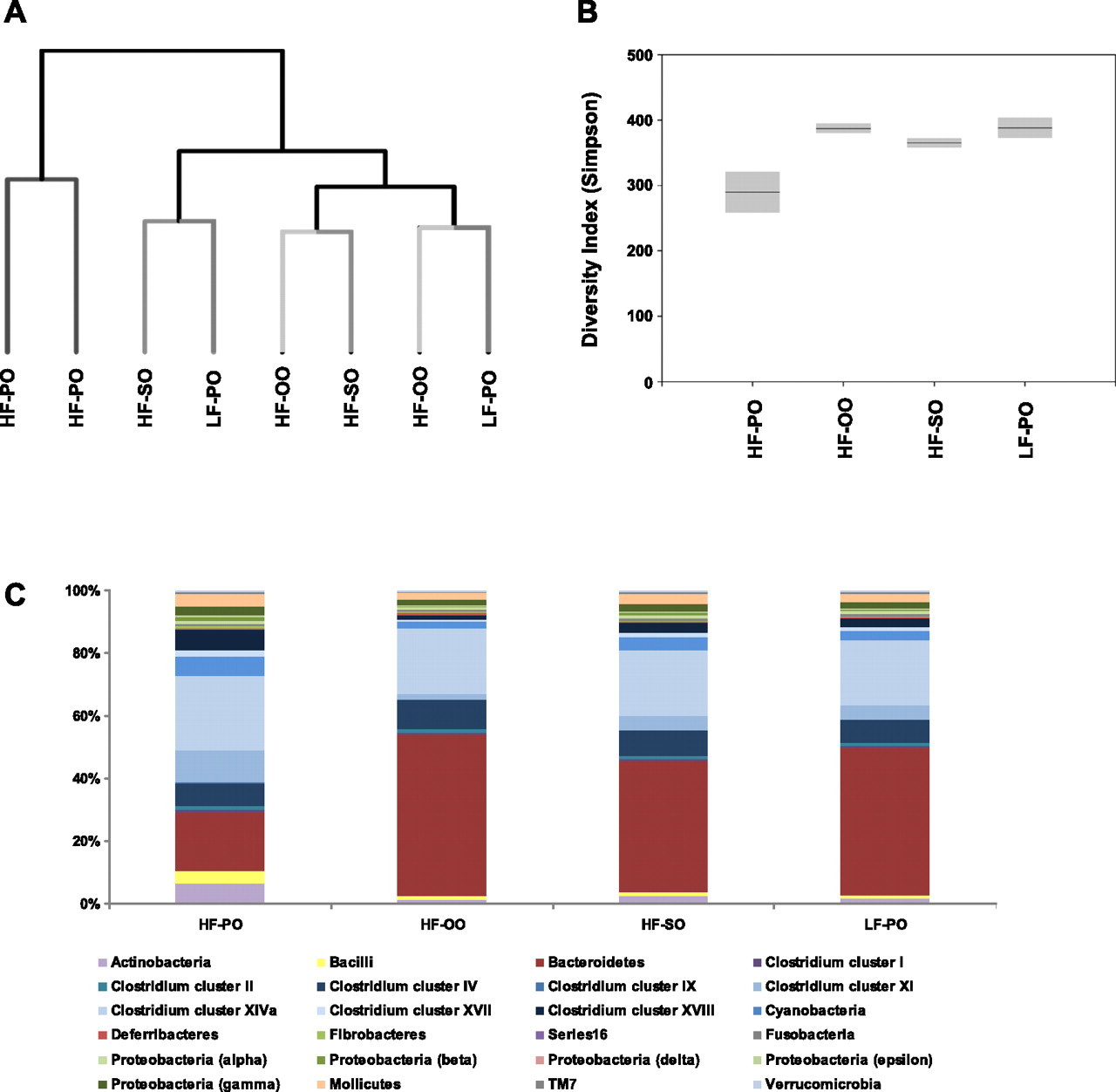
Consumption of soybean or olive oil at recommended concentrations increased the intestinal microbiota diversity and insulin sensitivity and prevented fatty liver compared to the effects of coconut oil
Author links open overlay panelValeriaLópez-Salazarab1Mónica SánchezTapiab1SandraTobón-CornejobDanielDíazcGabrielaAlemán-EscondrillasbOmarGranados-PortillobLiliaNoriegabArmando RTovarbNimbeTorresb
The Journal of Nutritional Biochemistry
Volume 94, August 2021, 108751Diets rich in mono or polyunsaturated fats have been associated with a healthy
phenotype, but there is controversial evidence about coconut oil (CO), which is rich
in saturated medium-chain fatty acids. Therefore, the purpose of the present work
was to study whether different types of oils rich in polyunsaturated (soybean oil,
SO), monounsaturated (olive oil, OO), or saturated fatty acids (coconut oil, CO)
can regulate the gut microbiota, insulin sensitivity, inflammation, mitochondrial
function in wild type and PPAR KO mice. The group that received SO showed the
highest microbial diversity, increase in Akkermansia muciniphila, high insulin
sensitivity and low grade inflammation, The OO group showed similar insulin
sensitivity and insulin signaling than SO, increase in Bifidobacterium, increase in
fatty acid oxidation and low grade inflammation. The CO consumption led to the
lowest bacterial diversity, a 9-fold increase in the LPS concentration leading to
metabolic endotoxemia, hepatic steatosis, increased lipogenesis, highest LDL-
cholesterol concentration and the lowest respiratory capacity and fatty acid
oxidation in the mitochondria. The absence of PPARdecreased alpha diversity
and increased LPS concentration particularly in the CO group, and increased
insulin sensitivity in the groups fed SO or OO. These results indicate that
consuming mono or polyunsaturated fatty acids produced health benefits at the
recommended intake but a high concentration of oils (three times the
recommended oil intake in rodents) significantly decreased the microbial alpha-
diversity independent of the type of oil.
"the results of the Western blot analysis revealed that
consuming 7% SO or 7% OO led to significantly lower TLR-4 and NF-kB protein
abundance than 7% CO, but the PPARKO mice showed a significant increase in
the abundance of these proteins, primarily in the group that received 21% CO"
"Increasing the % of dietary fat increased the serum
LPS concentration, but the consumption of 21% CO, increased the concentration
of LPS in the serum by 90-fold compared to the 7% SO group" (ouch
Discuss. Intersting points are:
- Increased TLR4 in coconut oil groups (@haidut )
- Decreased lactobacillus reuteri in coconut oil group. (This study showed the direct opposite)
- Lower bacterial diversity resulting in inflammation following coconut oil (@Amazoniac )
- Mice at 7% cocnut oil had higher BW gain compared to SO or OO, while 21% coconut oil made animals leaner.