ecstatichamster
Member
- Joined
- Nov 21, 2015
- Messages
- 10,504
Does peat mean that ACE2 is more effective thanks to the angiotensin receptor blockage or that ACE2 levels actually do increase? Does anyone have the quote?
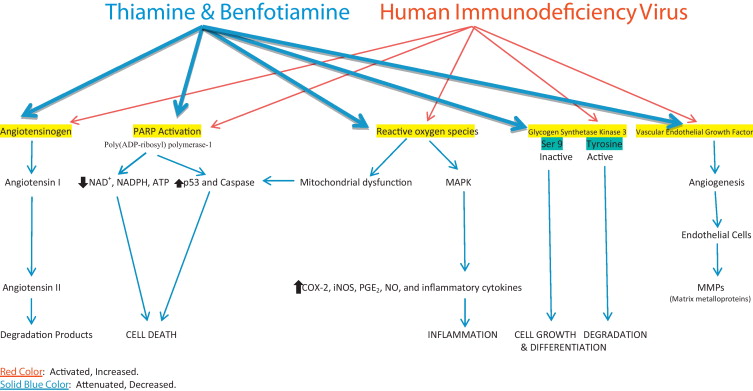
Most Likely Cure To Coronavirus Seems To Revolve Around Angiotensin