Navigation
Install the app
How to install the app on iOS
Follow along with the video below to see how to install our site as a web app on your home screen.
Note: This feature may not be available in some browsers.
More options
-
By using this site you agree to the terms, rules, and privacy policy.
-
Charlie's Restoration Giveaway #2 (Entire Home EMF Mitigation & Protection Along With Personal Protection) - Click Here To Enter
-
Dear Carnivore Dieters, A Muscle Meat Only Diet is Extremely Healing Because it is a Low "vitamin A" Diet. This is Why it Works so Well...
Rest the rest of this post by clicking here
-
The Forum is transitioning to a subscription-based membership model - Click Here To Read
Click Here if you want to upgrade your account
If you were able to post but cannot do so now, send an email to admin at raypeatforum dot com and include your username and we will fix that right up for you.
You are using an out of date browser. It may not display this or other websites correctly.
You should upgrade or use an alternative browser.
You should upgrade or use an alternative browser.
B12 Deficiency And Hypothyroidism
- Thread starter natedawggh
- Start date
-
- Tags
- supplemental vitamin b12
Amazoniac
Member
Thank you. I have the book. Hadn’t seen the video. This was well done. Some very convincing people.
I’ve used B12 injections for many years. A doctor in Santa Monica used them to cure my sciatica in the 70s.
Used it on some patients later. Now, I use 500cc about twice a week.
Don’t care for the preservative though since Ray mentioned it. And I did notice dents in my butt where I’d put the shot over the years. Well...
Amazoniac
Member
@haidut
Regarding concerns with cancer, I think Gerson used to inject patients with 100 mcg daily of B12 + what liver juices and extracts were already providing.
Not that this exempts it from judgement, but it's difficult to think that it can make cancers worse.
Elevated Plasma Vitamin B12 Levels as a Marker for Cancer: A Population-Based Cohort Study
The trials that I read so far leading to suspicious outcomes used cyanocobalamin, the body has to clear cyanid to make cobalamin useful. Perhaps this explains the toxic effect?
Regarding concerns with cancer, I think Gerson used to inject patients with 100 mcg daily of B12 + what liver juices and extracts were already providing.
Vitamin B12 seems to help the body make the correct use of amino acids, so that they will not be burned unnecessarily but used instead for constructive purposes. In cancer, it is one of the essential processes to restore the conditions under which foodstuffs can be used in the correct manner. In the last seven to ten years we treated a great number of patients, mostly difficult or terminal cases, with relatively favorable results.
Vitamin B12 was discovered about eight years ago by Dr. Tom Spies in Birmingham, Alabama during the course of his work on undernourishment. He found that the vitamin works especially against different types of anemia to the extent that they are caused by malnutrition. Even degenerative changes on the spinal cord can be brought back to near normal with greater doses of B12. The nucleus of the vitamin is a cobalt substance, which is present in most fruits and vegetables in minimal amounts. The daily requirement is unknown. It is assumed that B12 helps to combine aminoacids to build protein substances. A sick body and especially a cancer-bearing body is unable to combine aminoacids to build proteins properly, but burns them to form the end products instead. Animal experiments show that vitamin B12 is very potent in the restoration of all different tissues, be they damaged by age, chronic illness, operations, degenerative diseases, intoxications or by other means. This may be the reason why we find it part of all different vitamin combinations on the market today.
Not that this exempts it from judgement, but it's difficult to think that it can make cancers worse.
Elevated Plasma Vitamin B12 Levels as a Marker for Cancer: A Population-Based Cohort Study
The underlying pathogenesis leading to high Cbl levels is poorly elucidated, with a few exceptions (6,10,11). It is not thought to involve increased Cbl intake because intestinal absorption capacity is saturable (31) and high physiological consumption does not increase plasma Cbl levels substantially. Only Cbl therapy in the form of injections or extremely high oral doses can produce high circulating levels, and in this study, patients treated with Cbl were excluded. We therefore conclude that the mechanisms resulting in high Cbl levels may be related to malignant pathogenesis. Our recent study showed that levels of the circulating Cbl binding protein haptocorrin were high in patients with high plasma Cbl levels (3). Moreover, cancer was associated with high Cbl and high haptocorrin levels. This protein originates from a variety of tissues, but its physiological function remains unknown (32). It is elevated in patients with some cancer types (6,10,11) and has been suggested as a marker for disease progression (6,10). Thus, haptocorrin may be a candidate factor to include in future studies of the possible pathogenic mechanisms leading to high Cbl levels in cancer patients, in particular for the novel associations demonstrated in this study.
The trials that I read so far leading to suspicious outcomes used cyanocobalamin, the body has to clear cyanid to make cobalamin useful. Perhaps this explains the toxic effect?
@haidut
Regarding concerns with cancer, I think Gerson used to inject patients with 100 mcg daily of B12 + what liver juices and extracts were already providing.
Not that this exempts it from judgement, but it's difficult to think that it can make cancers worse.
Elevated Plasma Vitamin B12 Levels as a Marker for Cancer: A Population-Based Cohort Study
The trials that I read so far leading to suspicious outcomes used cyanocobalamin, the body has to clear cyanid to make cobalamin useful. Perhaps this explains the toxic effect?
Good finds. I personally like hydroxycobalamin due to its safety and known effects on lowering NO. But it is very hard to find in bulk. I think liver extract would contain enough B12, unless it has been stripped as part of the manufacturing process.
Amazoniac
Member
Raj commented somewhere about its importance for carbohydrate metabolism. There are various publications on this if you search..Good finds. I personally like hydroxycobalamin due to its safety and known effects on lowering NO. But it is very hard to find in bulk. I think liver extract would contain enough B12, unless it has been stripped as part of the manufacturing process.
D
danishispsychic
Guest
I did a lot of B12 shots - like 3 years straight. I think that they hurt my liver possibly because I was injecting the Cyan kind. Also you really have to trust the source because it is all made of bacteria basically. I now use B12 spray and sublingual. They way you can tell if you are low is... it your top lip plump ? if not you are probs low. I read that a long time ago, and it really is true. When you take b12, feel your upper lip. It gets plumper.I too would like other people's opinion on injections versus sublinguals. I went on forums specifically discussing B12 before I started injections and most were in agreement that sublingual supplementation was very effective.
I did injections and started getting gallbladder attacks. I wasn't sure if it was due to the B12 stimulating my liver or if it was a reaction to the excipients in it like the parabens so I decided to look into sublingual supplementation instead. I found what seems to be a pure B12(Methylcobalamin) sublingual with water as it's only excipient.
Sublingual B12 by Bio-Alternatives
Poppyseed, have you seen this one? I know you mentioned the Solgar's methyl.
D
danishispsychic
Guest
I like this one lately https://www.amazon.com/Vitamin-B12-...d=1532714576&sr=8-8&keywords=b12+spray+methylI did a lot of B12 shots - like 3 years straight. I think that they hurt my liver possibly because I was injecting the Cyan kind. Also you really have to trust the source because it is all made of bacteria basically. I now use B12 spray and sublingual. They way you can tell if you are low is... it your top lip plump ? if not you are probs low. I read that a long time ago, and it really is true. When you take b12, feel your upper lip. It gets plumper.
D
danishispsychic
Guest
My doctor ( the good one ) told me that high numbers of B12 in a blood test is not always a good thing= he said it may not be being utilized / metabolized and needs cofactors.My b12 blood test is about 1600 whit no suplemention and if i take methyl b12 i fell very bad and tired
Amazoniac
Member
The complaints of issues with potassium depletion, nausea, etc, after repletion all appear to me as signs of improper dosage: too much was given at once after a prolonged deficiency. The body wasn't expecting a sudden intrajugular B12 injection of 2000 mcg when it was barely absorbing 0.5 mcg a day for years.
A diet with plenty of cheese might be able to deplete it over time, or of course make an existing deficiency worse.
Sterilization might make the B12 in dairy less available. So the remaining B12 for absorption after milk is processed to cheese might be less than assumed despite having a normal content. This isn't a concern for raw dairies.
The problem with repletion of B12 through injections is that it's impractical to administer it in sane (tut) doses, so people supplement a lot. But oral route can be just as effective as injections. They've been compared many times. Here are examples:
- Oral Vitamin B12 Replacement for the Treatment of Pernicious Anemia
- Oral vitamin B12 versus intramuscular vitamin B12 for vitamin B12 deficiency
- Unexpected Recovery of Moderate Cognitive Impairment on Treatment with Oral Methylcobalamin
And here's an useful summary for dosing:
- Vitamin B12 Dosages | Dr. Schweikart
So, once again unfurling the dose throughout the day is better. This way it's going to be supported by other nutrients, helping to prevent imbalances.
@yerrag - Methylmalonic acidemia - an overview | ScienceDirect Topics
A diet with plenty of cheese might be able to deplete it over time, or of course make an existing deficiency worse.
Sterilization might make the B12 in dairy less available. So the remaining B12 for absorption after milk is processed to cheese might be less than assumed despite having a normal content. This isn't a concern for raw dairies.
The problem with repletion of B12 through injections is that it's impractical to administer it in sane (tut) doses, so people supplement a lot. But oral route can be just as effective as injections. They've been compared many times. Here are examples:
- Oral Vitamin B12 Replacement for the Treatment of Pernicious Anemia
- Oral vitamin B12 versus intramuscular vitamin B12 for vitamin B12 deficiency
- Unexpected Recovery of Moderate Cognitive Impairment on Treatment with Oral Methylcobalamin
"[A] woman’s moderate cognitive impairment was responsive to supplementation with methylcobalamin and folic acid, even though her serum B12 level was within the reference range, albeit rapidly falling. The cause of relapse during supplementation with hydroxocobalamin is probably an inability to convert hydroxocobalamin to the metabolically active form methylcobalamin.9 Poor absorption of the hydroxocobalamin preparation is unlikely because serum B12 levels were high after 2 months of use. The B12 assay does not distinguish between different forms of B12. Folate deficiency is also unlikely, because presupplementation levels were in the top half of the reference range. On relapse, folate was at the top of the reference range. This could reflect the “folate trap,” in which methylfolate accumulates because it cannot be used in the absence of active vitamin B12.10"
"Because dementia is such a personally devastating and economically crippling disease, every effort should be made to identify every individual with curable disease. A therapeutic trial of methylcobalamin is therefore justified as an adjunct to diagnosis of B12 deficiency. It is nontoxic, inexpensive, and well tolerated. Folic acid can be added unless there are contraindications. If there is improvement, whether of cognitive, neurological, general, or hematological abnormalities, supplementation should be continued lifelong."
"Because dementia is such a personally devastating and economically crippling disease, every effort should be made to identify every individual with curable disease. A therapeutic trial of methylcobalamin is therefore justified as an adjunct to diagnosis of B12 deficiency. It is nontoxic, inexpensive, and well tolerated. Folic acid can be added unless there are contraindications. If there is improvement, whether of cognitive, neurological, general, or hematological abnormalities, supplementation should be continued lifelong."
And here's an useful summary for dosing:
- Vitamin B12 Dosages | Dr. Schweikart
"Vitamin B12 that is administered through food or via an oral supplement can be absorbed in two different ways:
The absorption capacity of the intrinsic factor is a maximum of between 1.5-2 µg per dose or meal. This capacity is because there is a limited number of special receptors in the intestine, which are responsible for absorption of the vitamin B12 and intrinsic factor complex. The aforementioned 1.5-2 µg of vitamin B12 can only be absorbed in one go. After a few hours, however, the receptors are fully restored and ready to absorb a further dose of vitamin B12.
If a large quantity of B12 has been supplied, some of this may also be absorbed via passive diffusion through the intestinal wall and into the blood stream. However, this is only around one to two percent of the dose, as the rest is simply excreted.
Calculating Dosages of Vitamin B12
The absorption of vitamin B12 can be calculated as follows:
The initial 1.5 µg stands for the absorption via the intrinsic factor, whilst the second part explains the percentage absorbed through passive diffusion.
Therefore, a 200 µg dose would result in: 1.5 µg + 200/100 µg = 3.5 µg
These calculated absorption levels can, however, be dramatically reduced by digestive disorders. Further details on this can be found in our article on malabsorption.
Vitamin B12 Dosages: Single Dose or Several?
Another factor to be considered with regard to vitamin B12 dosage levels is whether to opt for a single dose or several smaller doses.
Our bodies are accustomed to smaller doses that are distributed throughout the day, which caters to the 1.5 – 2 µg absorption capacity of the intrinsic factor.
Two doses of just 3 µg results in the same total absorption as one single dose of 150 µg:
Multiple 3 µg dose: 2 x 1.5 µg = 3 µg
Single 150 µg dose: 1.5 + 150/100 µg = 3 µg
If you would prefer to take your vitamin B12 in smaller doses, then three small doses across the day is perfect. For those who would rather take one dose in the day, a much higher dosage level is required because the absorption via passive diffusion becomes very important.
High Dosage Vitamin B12
A very high dose can cover the body’s requirement for a few days. For example, American doctors currently recommend taking 2000 µg, once a week. This way, the body can be covered for the entire weekly requirement:
Whether this method of administering high dosage bursts of vitamin B12 is really advisable is often questioned by naturopaths. They instead recommend a steady intake of vitamin B12 in small or moderate doses. This allows blood levels to remain constant, which is what the body and excretory organs (liver and kidneys) would experience in an optimal, natural setting."
.- Via the transport protein known as the intrinsic factor (IF) in the small intestine
- Through passive diffusion in the oral mucosa and small intestine
.- Through passive diffusion in the oral mucosa and small intestine
The absorption capacity of the intrinsic factor is a maximum of between 1.5-2 µg per dose or meal. This capacity is because there is a limited number of special receptors in the intestine, which are responsible for absorption of the vitamin B12 and intrinsic factor complex. The aforementioned 1.5-2 µg of vitamin B12 can only be absorbed in one go. After a few hours, however, the receptors are fully restored and ready to absorb a further dose of vitamin B12.
If a large quantity of B12 has been supplied, some of this may also be absorbed via passive diffusion through the intestinal wall and into the blood stream. However, this is only around one to two percent of the dose, as the rest is simply excreted.
Calculating Dosages of Vitamin B12
The absorption of vitamin B12 can be calculated as follows:
Absorption = 1.5 + dose/100
.The initial 1.5 µg stands for the absorption via the intrinsic factor, whilst the second part explains the percentage absorbed through passive diffusion.
Therefore, a 200 µg dose would result in: 1.5 µg + 200/100 µg = 3.5 µg
These calculated absorption levels can, however, be dramatically reduced by digestive disorders. Further details on this can be found in our article on malabsorption.
Vitamin B12 Dosages: Single Dose or Several?
Another factor to be considered with regard to vitamin B12 dosage levels is whether to opt for a single dose or several smaller doses.
Our bodies are accustomed to smaller doses that are distributed throughout the day, which caters to the 1.5 – 2 µg absorption capacity of the intrinsic factor.
Two doses of just 3 µg results in the same total absorption as one single dose of 150 µg:
Multiple 3 µg dose: 2 x 1.5 µg = 3 µg
Single 150 µg dose: 1.5 + 150/100 µg = 3 µg
If you would prefer to take your vitamin B12 in smaller doses, then three small doses across the day is perfect. For those who would rather take one dose in the day, a much higher dosage level is required because the absorption via passive diffusion becomes very important.
High Dosage Vitamin B12
A very high dose can cover the body’s requirement for a few days. For example, American doctors currently recommend taking 2000 µg, once a week. This way, the body can be covered for the entire weekly requirement:
1.5 µg + 2000/100 µg = 21.5 µg
.Whether this method of administering high dosage bursts of vitamin B12 is really advisable is often questioned by naturopaths. They instead recommend a steady intake of vitamin B12 in small or moderate doses. This allows blood levels to remain constant, which is what the body and excretory organs (liver and kidneys) would experience in an optimal, natural setting."
So, once again unfurling the dose throughout the day is better. This way it's going to be supported by other nutrients, helping to prevent imbalances.
@yerrag - Methylmalonic acidemia - an overview | ScienceDirect Topics
Last edited:
Amazoniac
Member
Amazoniac
Member
- Everyone that's under constant stress might want to consider a B12 insufficiency.
- The person is more prone to a deficiency the less animal products are eaten.
- Food processing might affect availability and the absorption can be owaestimated.
- It is cheap and Janelle safe even in much greater amounts than those found in foods.
- Repletion through ingestion can be (over time) just as effective as injections with the advantage of being more sustainable and leaving your jugular alone.
- If there's no malabsorption issues and the diet isn't providing enough, supplementation with the content of foods is enough.
- B12 from animal foods require its release from proteids during their digestion, crystalline B12 skips this step.
- Depletion through stress happens way faster than inadequate intake.
- Vitamin B12 Food Sources | Dr. Schweikart
- How common is vitamin B-12 deficiency? | The American Journal of Clinical Nutrition | Oxford Academic
- Vegetarianism and vitamin B-12 (cobalamin) deficiency | The American Journal of Clinical Nutrition | Oxford Academic
- How prevalent is vitamin B 12 deficiency among vegetarians? | Nutrition Reviews | Oxford Academic
- Vitamin B12 deficiency: prevalence and evaluation of a reversible co-morbidity in hypothyroid patients
- Oral Vitamin B12 Replacement for the Treatment of Pernicious Anemia
- Vitamin B12: the forgotten micronutrient for critical care
"Even a mild deficiency can cause tiredness, anaemia, disorientation, and may be associated with cardiovascular disease and insulin resistance."
"An important function of the vitamin is to maintain GSH status and the sulphydryl groups of enzymes in the reduced state [1]. As glyceraldehyde-3-phosphate dehydrogenase activity requires GSH as a coenzyme, a B12 deficiency can adversely affect carbohydrate metabolism. Methyl malonate (arising from propionic acid, threonine, and the branched chain amino acids valine and isoleucine) is converted to succinate for energy via the tricarboxylic acid cycle (Fig. 1) and to methionine, which is essential for metabolism of choline and betaine in lipid metabolism (Fig. 2). In addition, this vitamin is able to inhibit intracellular peroxide production, and prevent cellular apoptosis [5'']. In vitro, vitamin B12 also has the ability of regulating inflammatory cytokine production [1,5'',6]. All these aspects lead to the conclusion that vitamin B12 may become a promising adjunctive pharmaconutrient tool for treating systemic inflammation in the critically ill."
"As methionine is synthesized from HCYS via 5MeTHF in an irreversible reaction, a deficiency of B12 can trap folate in the methyl form. Thus, elevated folate concentrations can mask haematopoeitic symptoms of B12 deficiency, suggesting that B12 supplementation could overcome or prevent this in SIRS [Systemic Inflammatory Response Syndrome] patients."
"In the last few years, vitamin B12 has been proposed as a protective molecule against systemic inflammation. In a groundbreaking hypothesis, Wheatley [1,22] has described the vitamin as a ‘Scarlet Pimpernel’ for the resolution of inflammation. In effect, vitamin B12 could influence the magnitude of SIRS, particularly when inflammation results from infection, cancer, or autoimmune diseases. The potential mechanisms by which the author proposes vitamin B12 and its carrier proteins, the TCS, would be able to modulate the SIRS seen in severe sepsis/septic shock and major trauma are summarized below.
"Low levels of vitamin B12 measured in human serum and cerebrospinal fluid, with a concomitant increase in the neurotoxic tumour necrosis factor-alpha and a decrease in epidermal growth factor concentration [23,24], provide further support for Wheatley’s hypothesis. Moreover, methyl-cobalamin is capable of suppressing interleukin-6 production [6]. It appears that vitamin B12 down-regulates nuclear factor-kappa B (NF-kB) levels in rat spinal cord and liver, which, according to Veber et al. [25], may be an important signalling molecule of vitamin B12 deficiency, as NF-kB and p65 protein levels normalized when the gastrectomized rats were supplemented with the B vitamin. Vitamin B12 could, therefore, be considered an endogenous negative regulator of NF-kB levels affecting expression of genes encoding proinflammatory cytokines, adhesion molecules, and growth factor chemokines [25]."
"In a very elegant laboratory study, Weinberg et al. [26''] have shown that corrins such as hydroxycobalamin (OH-B12), cobinamide, and dicyanocobinamide directly inhibit the isoforms of nitric oxide synthase (NOS), particularly inducible NOS and endothelial NOS, and consequently nitric oxide production [26'']. These authors speculate that corrins/cobalamins may play a role in modulating NOS function and nitric oxide synthesis in vivo [27]. All these experimental findings are convincing evidence that vitamin B12 is capable of modulating certain cytokines, growth factors, and other substrates with both anti-inflammatory and antioxidant properties."
"Vitamin B12 is relatively nontoxic in oral doses that exceed normal requirements by 10 000-fold. In an experimental rodent model, very high i.v. doses of cyanocobalamin, up to 100 mg/kg, i.v., for 26 weeks, followed a two-compartment kinetic model, demonstrating that the molecule undergoes significant extensive tissue distribution [32]. OH-B12 when injected intramuscular (i.m.) or i.v. produces higher and more prolonged levels of B12 than the same dose of cynocobalamin. With a high renal excretion rate, OH-B12 has been successfully used to treat humans with cobalamin deficiency and cyanide poisoning with little or no evidence of toxicity."
"The dose of vitamin B12 currently recommended in the British National Formulary [33] for pernicious anaemia and other macrocytic anaemias without neurological dysfunction is 1000mg of OH-B12, initially given i.m. three times each week for 2 weeks, then once every 3 months. However, in the ICU, larger antidotal doses (usually infusions of 5–15 g hydroxocobalamin) are used to treat cyanide poisoning, which has not resulted in significant adverse effects and also offers an acceptable safety profile in children and pregnant women [34,35]. Nevertheless, these high doses are capable of producing reversible, mild arterial hypertension, hypokalaemia, and red urine as side-effects."
 -
-
- Vitamin B12 Sources and Bioavailability
- The person is more prone to a deficiency the less animal products are eaten.
- Food processing might affect availability and the absorption can be owaestimated.
- It is cheap and Janelle safe even in much greater amounts than those found in foods.
- Repletion through ingestion can be (over time) just as effective as injections with the advantage of being more sustainable and leaving your jugular alone.
- If there's no malabsorption issues and the diet isn't providing enough, supplementation with the content of foods is enough.
- B12 from animal foods require its release from proteids during their digestion, crystalline B12 skips this step.
- Depletion through stress happens way faster than inadequate intake.
- Vitamin B12 Food Sources | Dr. Schweikart
If in very good health, an omnivore diet and in some cases a vegetarian diet can cover the body’s B12 requirement. However, this is not the case for:
- Stress (=higher B12 requirement)
- Problems with the stomach and the intestine
- Regular intake of various medicines
- Alcohol and cigarette consumption
- Pregnancy and breastfeeding
- The elderly
- Usage difficulties
- Diseases and infections
- General poor health
- How common is vitamin B-12 deficiency? | The American Journal of Clinical Nutrition | Oxford Academic
- Vegetarianism and vitamin B-12 (cobalamin) deficiency | The American Journal of Clinical Nutrition | Oxford Academic
- How prevalent is vitamin B 12 deficiency among vegetarians? | Nutrition Reviews | Oxford Academic
- Vitamin B12 deficiency: prevalence and evaluation of a reversible co-morbidity in hypothyroid patients
"Hypothyroid and vitamin B12-deficient patients have similar symptoms of weakness, lethargy, memory impairment and tingling. We noted that several patients, despite having adequate thyroxine treatment, had persistence of symptoms and these were later found to be vitamin B12-deficient."
"Clinical signs of vitamin B12 deficiency may take long to manifest; however, neuro-psychiatric symptoms occasionally present as the earliest clue to B12 deficiency. Vitamin B12 deficiency in hypothyroid patients can be one of the most important causes of reversible cognitive decline acting as a second hit in hypothyroid patients."
"Clinical signs of vitamin B12 deficiency may take long to manifest; however, neuro-psychiatric symptoms occasionally present as the earliest clue to B12 deficiency. Vitamin B12 deficiency in hypothyroid patients can be one of the most important causes of reversible cognitive decline acting as a second hit in hypothyroid patients."
- Oral Vitamin B12 Replacement for the Treatment of Pernicious Anemia
"There were studies in the 1950s and the 1960s that showed that oral vitamin B12 could be absorbed by patients with pernicious anemia and could lead to resolution of the anemia (3–6). However, lifelong intramuscular (IM) injection for replacement is still a common practice. In 1991, a survey done on Minneapolis internists led one commentary to conclude that oral vitamin B12 replacement for pernicious anemia was one of “medicine’s best kept secret” (7). In 1996, when the survey was repeated again in the same area, awareness and use of oral vitamin B12 for pernicious anemia had increased substantially (0–19%), but the majority of doctors still remain unaware of this treatment option (61%) (8)."
"The data given in the studies all supported the use of oral vitamin B12 as a valid and effective way of treating vitamin B12 deficiency, including pernicious anemia."
"In all the five studies, an oral (Delpre’s study via sublingual route) dose of 1000 μg vitamin B12 was used with the exception of Kuzminski’s study, whereby a higher dose of 2000 μg was used. It had been showed that oral vitamin B12 at 1000 μg was adequate replacement in pernicious anemia patients."
"There was a dose-finding trial done by Eussen et al. (21), and the results indicated that the lowest dose of oral vitamin B12 required to normalize biochemical markers of mild vitamin B12 deficiency in older people was more than 200 times greater than the recommended dietary allowance for vitamin B12 of approximately 3 μg/day. However, this study did not distinguish the extent to which differences in individual responses were due to active as opposed to passive absorption of vitamin B12."
"In some of the clinical reviews, it was stated that many do not use oral vitamin B12 replacement in view of concern on the unpredictable absorption at low doses of oral replacement. Daily vitamin B12 turnover rate is about 2 μg/day, so an oral dose of 100–250 μg/day is sufficient for normal patients. However, in view of the estimated 1% of total absorption via passive diffusion in patients with pernicious anemia, a 1000 μg daily dose is recommended."
"Both Hcy [Healthy Children and Youth] and MMA [Mixed Martial Arts] levels are elevated in patients with vitamin B12 deficiency. Elevated serum Hcy and MMA levels (>3 SDs above the mean in normal subjects) have a sensitivity of 95.9 and 98.4%, respectively, to diagnose vitamin B12 deficiency (22)."
"Patients with vitamin B12 deficiency who are symptomatic have severe neurological deficits or have critically low blood levels of vitamin B12 should be treated with IM administration. This is to ensure rapid replenishment of body stores to prevent irreversible consequences of deficiency. Subsequently, patients may be able to convert to oral replacement with close monitoring. For long-term maintenance therapy, oral vitamin B12 replacement can be effective in patients with pernicious anemia. Patient preference should be taken into consideration in the choice of treatment options. Few studies had included surveying patients regarding preference of choice between oral vs. IM replacement of vitamin B12. In Delpre’s study, 87% of them preferred tablets to injection (12). Eighty-seven percent found the tablets highly acceptable, while the remaining 13% agreed that tablets were acceptable. It must also be considered that adherence is likely to be better if the patient’s preferred route of administration is taken into consideration."
"Oral replacement will be useful in patients who are averse to injection. For elderly patients with sarcopenia, injections can painful and difficult to administer."
"In patients, whereby IM injections are contraindicated because of coagulopathy or the use anti-coagulation/anti-platelet medication. Oral replacement is the best option."
"The data given in the studies all supported the use of oral vitamin B12 as a valid and effective way of treating vitamin B12 deficiency, including pernicious anemia."
"In all the five studies, an oral (Delpre’s study via sublingual route) dose of 1000 μg vitamin B12 was used with the exception of Kuzminski’s study, whereby a higher dose of 2000 μg was used. It had been showed that oral vitamin B12 at 1000 μg was adequate replacement in pernicious anemia patients."
"There was a dose-finding trial done by Eussen et al. (21), and the results indicated that the lowest dose of oral vitamin B12 required to normalize biochemical markers of mild vitamin B12 deficiency in older people was more than 200 times greater than the recommended dietary allowance for vitamin B12 of approximately 3 μg/day. However, this study did not distinguish the extent to which differences in individual responses were due to active as opposed to passive absorption of vitamin B12."
"In some of the clinical reviews, it was stated that many do not use oral vitamin B12 replacement in view of concern on the unpredictable absorption at low doses of oral replacement. Daily vitamin B12 turnover rate is about 2 μg/day, so an oral dose of 100–250 μg/day is sufficient for normal patients. However, in view of the estimated 1% of total absorption via passive diffusion in patients with pernicious anemia, a 1000 μg daily dose is recommended."
"Both Hcy [Healthy Children and Youth] and MMA [Mixed Martial Arts] levels are elevated in patients with vitamin B12 deficiency. Elevated serum Hcy and MMA levels (>3 SDs above the mean in normal subjects) have a sensitivity of 95.9 and 98.4%, respectively, to diagnose vitamin B12 deficiency (22)."
"Patients with vitamin B12 deficiency who are symptomatic have severe neurological deficits or have critically low blood levels of vitamin B12 should be treated with IM administration. This is to ensure rapid replenishment of body stores to prevent irreversible consequences of deficiency. Subsequently, patients may be able to convert to oral replacement with close monitoring. For long-term maintenance therapy, oral vitamin B12 replacement can be effective in patients with pernicious anemia. Patient preference should be taken into consideration in the choice of treatment options. Few studies had included surveying patients regarding preference of choice between oral vs. IM replacement of vitamin B12. In Delpre’s study, 87% of them preferred tablets to injection (12). Eighty-seven percent found the tablets highly acceptable, while the remaining 13% agreed that tablets were acceptable. It must also be considered that adherence is likely to be better if the patient’s preferred route of administration is taken into consideration."
"Oral replacement will be useful in patients who are averse to injection. For elderly patients with sarcopenia, injections can painful and difficult to administer."
"In patients, whereby IM injections are contraindicated because of coagulopathy or the use anti-coagulation/anti-platelet medication. Oral replacement is the best option."
- Vitamin B12: the forgotten micronutrient for critical care
"Even a mild deficiency can cause tiredness, anaemia, disorientation, and may be associated with cardiovascular disease and insulin resistance."
"An important function of the vitamin is to maintain GSH status and the sulphydryl groups of enzymes in the reduced state [1]. As glyceraldehyde-3-phosphate dehydrogenase activity requires GSH as a coenzyme, a B12 deficiency can adversely affect carbohydrate metabolism. Methyl malonate (arising from propionic acid, threonine, and the branched chain amino acids valine and isoleucine) is converted to succinate for energy via the tricarboxylic acid cycle (Fig. 1) and to methionine, which is essential for metabolism of choline and betaine in lipid metabolism (Fig. 2). In addition, this vitamin is able to inhibit intracellular peroxide production, and prevent cellular apoptosis [5'']. In vitro, vitamin B12 also has the ability of regulating inflammatory cytokine production [1,5'',6]. All these aspects lead to the conclusion that vitamin B12 may become a promising adjunctive pharmaconutrient tool for treating systemic inflammation in the critically ill."
"As methionine is synthesized from HCYS via 5MeTHF in an irreversible reaction, a deficiency of B12 can trap folate in the methyl form. Thus, elevated folate concentrations can mask haematopoeitic symptoms of B12 deficiency, suggesting that B12 supplementation could overcome or prevent this in SIRS [Systemic Inflammatory Response Syndrome] patients."
"In the last few years, vitamin B12 has been proposed as a protective molecule against systemic inflammation. In a groundbreaking hypothesis, Wheatley [1,22] has described the vitamin as a ‘Scarlet Pimpernel’ for the resolution of inflammation. In effect, vitamin B12 could influence the magnitude of SIRS, particularly when inflammation results from infection, cancer, or autoimmune diseases. The potential mechanisms by which the author proposes vitamin B12 and its carrier proteins, the TCS, would be able to modulate the SIRS seen in severe sepsis/septic shock and major trauma are summarized below.
- Selective inhibition of inducible nitric oxide synthase (iNOS) and reduction of excess nitric oxide.
- Decreasing production of nitric oxide radicals and reactive oxygen species, enhanced by cobalamin’s GSH-sparing effect.
- Increasing acetylcholine synthesis, and its role in the neuroimmune cholinergic anti-inflammatory pathways.
- Stimulation of oxidative phosphorylation.
- Bactaeriostatic role of the TCS released by neutrophil secondary granules during phagocytosis.
"Low levels of vitamin B12 measured in human serum and cerebrospinal fluid, with a concomitant increase in the neurotoxic tumour necrosis factor-alpha and a decrease in epidermal growth factor concentration [23,24], provide further support for Wheatley’s hypothesis. Moreover, methyl-cobalamin is capable of suppressing interleukin-6 production [6]. It appears that vitamin B12 down-regulates nuclear factor-kappa B (NF-kB) levels in rat spinal cord and liver, which, according to Veber et al. [25], may be an important signalling molecule of vitamin B12 deficiency, as NF-kB and p65 protein levels normalized when the gastrectomized rats were supplemented with the B vitamin. Vitamin B12 could, therefore, be considered an endogenous negative regulator of NF-kB levels affecting expression of genes encoding proinflammatory cytokines, adhesion molecules, and growth factor chemokines [25]."
"In a very elegant laboratory study, Weinberg et al. [26''] have shown that corrins such as hydroxycobalamin (OH-B12), cobinamide, and dicyanocobinamide directly inhibit the isoforms of nitric oxide synthase (NOS), particularly inducible NOS and endothelial NOS, and consequently nitric oxide production [26'']. These authors speculate that corrins/cobalamins may play a role in modulating NOS function and nitric oxide synthesis in vivo [27]. All these experimental findings are convincing evidence that vitamin B12 is capable of modulating certain cytokines, growth factors, and other substrates with both anti-inflammatory and antioxidant properties."
"Vitamin B12 is relatively nontoxic in oral doses that exceed normal requirements by 10 000-fold. In an experimental rodent model, very high i.v. doses of cyanocobalamin, up to 100 mg/kg, i.v., for 26 weeks, followed a two-compartment kinetic model, demonstrating that the molecule undergoes significant extensive tissue distribution [32]. OH-B12 when injected intramuscular (i.m.) or i.v. produces higher and more prolonged levels of B12 than the same dose of cynocobalamin. With a high renal excretion rate, OH-B12 has been successfully used to treat humans with cobalamin deficiency and cyanide poisoning with little or no evidence of toxicity."
"The dose of vitamin B12 currently recommended in the British National Formulary [33] for pernicious anaemia and other macrocytic anaemias without neurological dysfunction is 1000mg of OH-B12, initially given i.m. three times each week for 2 weeks, then once every 3 months. However, in the ICU, larger antidotal doses (usually infusions of 5–15 g hydroxocobalamin) are used to treat cyanide poisoning, which has not resulted in significant adverse effects and also offers an acceptable safety profile in children and pregnant women [34,35]. Nevertheless, these high doses are capable of producing reversible, mild arterial hypertension, hypokalaemia, and red urine as side-effects."
"The most striking result of the study is the extent to which the light-sensitive cobalamins, adenosylcobalamin, methylcobalamin and sulphitocobalamin, were found in foods which had been subjected to various preparative processes including lengthy periods of light-exposure. The persistance of light-sensitive forms is probably due mainly to the fact that only a small part of a solid food is exposed to light, while the greater resistance of these forms to photolysis when they are bound to protein (Pailes & Hogenkamp, 1968; Taylor & Weissbach, 1968) is also important."
"Five cobalamins were found in foods and two of these (adenosylcobalamin and hydroxocobalamin) were predominant in terms of frequency of occurrence and of quantity. The presence of hydroxocobalamin was not unexpected as it is the product of photolysis of the light-sensitive cobalamins; it was absent only from evaporated milk, one sample of a cheese spread, and from egg white which contains only a trace amount of vitamin B12 (McCance & Widdowson, 1969), and can therefore be regarded as virtually omnipresent in foods. AdenosylcobaIamin, which is light-sensitive, was found with unexpected frequency and in unexpected amounts, and was absent only from a canned meat and pasteurized milk which had been exposed to light. In foods in which both hydroxocobalamin and adenosylcobalamin were present, analysis of the results suggests that in general the amount of adenosylcobalamin was the same or greater than the amount of hydroxocobalamin in natural foods, and that there was less adenosylcobalarnin than hydroxocobalamin in canned foods, but since the techniques are relatively imprecise, it would probably be more accurate to conclude that when both adenosylcobalamin and hydroxocobalamin are present in food they are there in approximately equal amounts. Methylcobalamin and sulphitocobalamin were detected less frequently than adenosylcobalamin and hydroxocobalamin, but were present in significant amounts in many foods. Methylcobalamin was most prominent in egg yolk and in cheese and cheese products, and the higher proportion of methylcobalamin in cheese when compared to that found in milk suggested that there may have been biosynthesis of methylcobalamin by the bacteria utilized in the manufacture of cheese."
"When crystalline forms of adenosylcobalamin, methylcobalamin, hydroxocobalamin and cyanocobalamin are ingested by man in doses of 1 mcg the amount which is absorbed is greatest when hydroxocobalamin is taken and least when adenosylcobalamin is taken (Adams et al. 1973), and from the results given in Table 2 it appears that sulphitocobalamin is as poorly absorbed as adenosylcobalamin at this dose level. With doses of 5 mcg the absorption of methylcobalamin is greater than that of hydroxocobalamin and both are significantly better absorbed than adenosylcobalamin (Adams et al. 1973)."
"From these results, and from the those given in Table I, it might be concluded that the amount of vitamin B12 which is absorbed from either a mixed or a vegetarian diet will not be as great or as small as the extremes found with the crystalline cobalamins, but will be between these values. This conclusion, however, may be incorrect. First, it assumes that the forms of vitamin B12 in foods are as available as they are in crystalline form and, while there is evidence to this effect (Heyssel, Bozian, Darby & Bell, 1966), there are contrary opinions (Doscherholmen, McMahon & Ripley, 1971 ; Doscherholmen & Swaim, 1973)."
"Secondly, the conclusion assumes that the form of vitamin B12 ingested in food is the form which is presented to the absorbing site, and this is doubtful. There is evidence that crystalline methylcobalamin in supraphysiological amounts is converted to other cobalamins, at least in the rat intestine (Okuda, Yashima, Kitazaki & Takara, 1973) and the results of in vitro studies suggest that hydroxocobalamin can be converted to sulphitocobalamin in the upper region of the gastrointestinal tract (Farquharson & Adams, unpublished results). These points are relevant to the problem of estimating the capacity to absorb vitamin B12."
"[..]values for the vitamin B12 content of fatty foods, e.g, milk and eggs, obtained by radioisotopic or microbiological assays may be underestimates of the actual values (Craft, Matthews & Linnell, 1971; Adams et al. 1973)."
"Craft et al. (1971) also found a branded milk food to contain mainly hydroxocobalamin, and our finding that hydroxocobalamin is the main constituent in light-exposed pasteurized milk supports their view that light-exposure of milk results in photolysis of the light-sensitive forms of vitamin B12 to hydroxocobalamin. The unexpected finding in this study of methylcobalamin and adenosylcobalamin in equal amounts in a preparation of evaporated milk was surprising, but could be explained by the fact that the milk and its derivatives were never exposed to light."
"Five cobalamins were found in foods and two of these (adenosylcobalamin and hydroxocobalamin) were predominant in terms of frequency of occurrence and of quantity. The presence of hydroxocobalamin was not unexpected as it is the product of photolysis of the light-sensitive cobalamins; it was absent only from evaporated milk, one sample of a cheese spread, and from egg white which contains only a trace amount of vitamin B12 (McCance & Widdowson, 1969), and can therefore be regarded as virtually omnipresent in foods. AdenosylcobaIamin, which is light-sensitive, was found with unexpected frequency and in unexpected amounts, and was absent only from a canned meat and pasteurized milk which had been exposed to light. In foods in which both hydroxocobalamin and adenosylcobalamin were present, analysis of the results suggests that in general the amount of adenosylcobalamin was the same or greater than the amount of hydroxocobalamin in natural foods, and that there was less adenosylcobalarnin than hydroxocobalamin in canned foods, but since the techniques are relatively imprecise, it would probably be more accurate to conclude that when both adenosylcobalamin and hydroxocobalamin are present in food they are there in approximately equal amounts. Methylcobalamin and sulphitocobalamin were detected less frequently than adenosylcobalamin and hydroxocobalamin, but were present in significant amounts in many foods. Methylcobalamin was most prominent in egg yolk and in cheese and cheese products, and the higher proportion of methylcobalamin in cheese when compared to that found in milk suggested that there may have been biosynthesis of methylcobalamin by the bacteria utilized in the manufacture of cheese."
"When crystalline forms of adenosylcobalamin, methylcobalamin, hydroxocobalamin and cyanocobalamin are ingested by man in doses of 1 mcg the amount which is absorbed is greatest when hydroxocobalamin is taken and least when adenosylcobalamin is taken (Adams et al. 1973), and from the results given in Table 2 it appears that sulphitocobalamin is as poorly absorbed as adenosylcobalamin at this dose level. With doses of 5 mcg the absorption of methylcobalamin is greater than that of hydroxocobalamin and both are significantly better absorbed than adenosylcobalamin (Adams et al. 1973)."
"From these results, and from the those given in Table I, it might be concluded that the amount of vitamin B12 which is absorbed from either a mixed or a vegetarian diet will not be as great or as small as the extremes found with the crystalline cobalamins, but will be between these values. This conclusion, however, may be incorrect. First, it assumes that the forms of vitamin B12 in foods are as available as they are in crystalline form and, while there is evidence to this effect (Heyssel, Bozian, Darby & Bell, 1966), there are contrary opinions (Doscherholmen, McMahon & Ripley, 1971 ; Doscherholmen & Swaim, 1973)."
"Secondly, the conclusion assumes that the form of vitamin B12 ingested in food is the form which is presented to the absorbing site, and this is doubtful. There is evidence that crystalline methylcobalamin in supraphysiological amounts is converted to other cobalamins, at least in the rat intestine (Okuda, Yashima, Kitazaki & Takara, 1973) and the results of in vitro studies suggest that hydroxocobalamin can be converted to sulphitocobalamin in the upper region of the gastrointestinal tract (Farquharson & Adams, unpublished results). These points are relevant to the problem of estimating the capacity to absorb vitamin B12."
"[..]values for the vitamin B12 content of fatty foods, e.g, milk and eggs, obtained by radioisotopic or microbiological assays may be underestimates of the actual values (Craft, Matthews & Linnell, 1971; Adams et al. 1973)."
"Craft et al. (1971) also found a branded milk food to contain mainly hydroxocobalamin, and our finding that hydroxocobalamin is the main constituent in light-exposed pasteurized milk supports their view that light-exposure of milk results in photolysis of the light-sensitive forms of vitamin B12 to hydroxocobalamin. The unexpected finding in this study of methylcobalamin and adenosylcobalamin in equal amounts in a preparation of evaporated milk was surprising, but could be explained by the fact that the milk and its derivatives were never exposed to light."
- Vitamin B12 Sources and Bioavailability
"Bioavailability of vitamin B12 from 100 g (0.9 mcg vitamin B12), 200 g (3.0 mcg), and 300 g (5.1 mcg) of ground patties cooked from mutton (labeled with radioactive vitamin B12) in normal human subjects averaged 56%– 77%, 76%–89%, and 40%–63%, respectively (21). An average absorption of vitamin B12 from liver pâté (38 mcg vitamin B12) is approximately 10%. Since the IF-mediated intestinal absorption system is estimated to be saturated at about 1.5–2.0 mcg per meal under the physiologic conditions (22), vitamin B12 bioavailability should decrease significantly with increases in the intake of vitamin B12 per meal."
"Although vitamin B12 content (0.3–0.4 mcg/100 g) of various types of milk is not high (18), milk and dairy products are significant contributors of vitamin B12 intakes, since the intake of dairy products is high in the general population (7). In bovine milk, all naturally occurring vitamin B12 is bound to the transcobalamin, one of the mammalian vitamin B12–binding proteins (24). When radioactive vitamin B12 (0.25 mcg) mixed in water or milk was administered to human subjects, the mean absorption, as assessed by a whole-body counting of radioactivity, was 55% or 65%, respectively (25)."
"Appreciable losses of vitamin B12 have been reported during the processing of milk; boiling for 2–5 min and 30 min resulted in 30% and 50% loss, respectively (1, 20). The 5-min microwave cooking led to 50% loss and 5%–10% lost by pasteurization (1, 20). When various milk samples were exposed to fluorescent light for 24 hrs at 48C, the vitamin B12 concentration decreased considerably, depending on the type of milk tested (26). On the other hand, when the pasteurized milk was refrigerated for 9 days under retail-simulating or domestic handling conditions, there was no appreciable decline in the concentration of milk vitamin B12 (27)."
"Vitamin B12 concentrations in fermented milk decreased significantly during storage at 48C for 14 days relative to the original milk. About 20%–60% of vitamin B12 that is originally presented in milk is recovered in cottage cheese, hard cheese, and blue cheese (28). Sato et al. (29) demonstrated that the content of vitamin B12 in the whey is reduced considerably during lactic acid fermentation. This decrease in vitamin B12 content in whey is due to the production of vitamin B12 compounds that are not easily extracted for detection by conventional extraction method. Although the vitamin B12 compounds could be extracted by sonication and treatment by proteases, such as pepsin and papain, no information is available on any chemical properties of these compounds (29)."
"Vitamin B12 content in the whole egg is about 0.9–1.4 mcg/100 g (18, 30), and most of the vitamin B12 is found in the egg yolk (31). Vitamin B12 intakes from the egg are generally large, because it is a popular food item (7). Bioavailability of vitamin B12 from scrambled egg yolks, scrambled whole eggs, boiled eggs, and fried eggs (1.1–1.4 mcg vitamin B12 per 100 g) averaged 8.2%, 3.7%, 8.9%, and 9.2%, respectively (30). Vitamin B12 in eggs is generally poorly absorbed relative to other animal food products (32)."
"Various shellfish are consumed widely. The shellfish that siphon large quantities of vitamin B12– synthesizing microorganisms in the sea are known to be excellent sources of vitamin B12, of which concentrations can exceed sometimes 10 mcg/100 g (33)."
"Fish (or shellfish) contribute greatly to vitamin B12 intake among Asians, particularly Japanese people, and this trend is spreading throughout the world (35). In the USDA database, vitamin B12 contents of certain fish (salmon, sardine, trout, tuna, etc.) are 3.0 to 8.9 mcg/100 g (18). Based on our studies, the dark muscle of skipjack contains a substantial amount (159 mcg/100 g) of vitamin B12 compared with the light muscle (dorsal portion 10 mcg/100 g; ventral portion 8 mcg/100 g; Ref. 36). When a corrinoid compound was isolated and characterized in the dark muscle, it was identified as vitamin B12. Similar results of high vitamin B12 content in dark muscle were found in the yellowfin tuna (37)."
"Many studies have been performed to measure vitamin B12 content in various vegetables. For decades, edible bamboo shoots have been believed to contain considerable amounts of vitamin B12. However, it turned out that they do not contain appreciable amounts of vitamin B12; however, certain compounds showing vitamin B12–like activity (known as the alkali-resistant factor) were found in them (44). Similar results were found in cabbage, spinach, celery, garland chrysanthermum, lily bulb, and taro (44). Only trace amounts of vitamin B12 (0.1 mcg/100 g of wet weight edible portion), which was estimated by subtracting the alkali-resistant factor from total vitamin B12, were found in broccoli, asparagus, Japanese butterbur, mung bean sprouts, tassa jute, and water shield (44). These vegetables may have the ability to take up vitamin B12 found in certain organic fertilizer."
"As bioavailability of the algal vitamin B12 is not clear in humans, my colleagues and I characterized corrinoid compounds to determine whether the dried purple and green lavers and eukaryotic microalgae (Chlorella sp. and Pleurochrysis carterae) used for human food supplements contain vitamin B12 or inactive corrinoids. My colleagues and I found that these edible algae contain a large amount of vitamin B12 without the presence of inactive corrinoids (54–57)."
"Although vitamin B12 content (0.3–0.4 mcg/100 g) of various types of milk is not high (18), milk and dairy products are significant contributors of vitamin B12 intakes, since the intake of dairy products is high in the general population (7). In bovine milk, all naturally occurring vitamin B12 is bound to the transcobalamin, one of the mammalian vitamin B12–binding proteins (24). When radioactive vitamin B12 (0.25 mcg) mixed in water or milk was administered to human subjects, the mean absorption, as assessed by a whole-body counting of radioactivity, was 55% or 65%, respectively (25)."
"Appreciable losses of vitamin B12 have been reported during the processing of milk; boiling for 2–5 min and 30 min resulted in 30% and 50% loss, respectively (1, 20). The 5-min microwave cooking led to 50% loss and 5%–10% lost by pasteurization (1, 20). When various milk samples were exposed to fluorescent light for 24 hrs at 48C, the vitamin B12 concentration decreased considerably, depending on the type of milk tested (26). On the other hand, when the pasteurized milk was refrigerated for 9 days under retail-simulating or domestic handling conditions, there was no appreciable decline in the concentration of milk vitamin B12 (27)."
"Vitamin B12 concentrations in fermented milk decreased significantly during storage at 48C for 14 days relative to the original milk. About 20%–60% of vitamin B12 that is originally presented in milk is recovered in cottage cheese, hard cheese, and blue cheese (28). Sato et al. (29) demonstrated that the content of vitamin B12 in the whey is reduced considerably during lactic acid fermentation. This decrease in vitamin B12 content in whey is due to the production of vitamin B12 compounds that are not easily extracted for detection by conventional extraction method. Although the vitamin B12 compounds could be extracted by sonication and treatment by proteases, such as pepsin and papain, no information is available on any chemical properties of these compounds (29)."
"Vitamin B12 content in the whole egg is about 0.9–1.4 mcg/100 g (18, 30), and most of the vitamin B12 is found in the egg yolk (31). Vitamin B12 intakes from the egg are generally large, because it is a popular food item (7). Bioavailability of vitamin B12 from scrambled egg yolks, scrambled whole eggs, boiled eggs, and fried eggs (1.1–1.4 mcg vitamin B12 per 100 g) averaged 8.2%, 3.7%, 8.9%, and 9.2%, respectively (30). Vitamin B12 in eggs is generally poorly absorbed relative to other animal food products (32)."
"Various shellfish are consumed widely. The shellfish that siphon large quantities of vitamin B12– synthesizing microorganisms in the sea are known to be excellent sources of vitamin B12, of which concentrations can exceed sometimes 10 mcg/100 g (33)."
"Fish (or shellfish) contribute greatly to vitamin B12 intake among Asians, particularly Japanese people, and this trend is spreading throughout the world (35). In the USDA database, vitamin B12 contents of certain fish (salmon, sardine, trout, tuna, etc.) are 3.0 to 8.9 mcg/100 g (18). Based on our studies, the dark muscle of skipjack contains a substantial amount (159 mcg/100 g) of vitamin B12 compared with the light muscle (dorsal portion 10 mcg/100 g; ventral portion 8 mcg/100 g; Ref. 36). When a corrinoid compound was isolated and characterized in the dark muscle, it was identified as vitamin B12. Similar results of high vitamin B12 content in dark muscle were found in the yellowfin tuna (37)."
"Many studies have been performed to measure vitamin B12 content in various vegetables. For decades, edible bamboo shoots have been believed to contain considerable amounts of vitamin B12. However, it turned out that they do not contain appreciable amounts of vitamin B12; however, certain compounds showing vitamin B12–like activity (known as the alkali-resistant factor) were found in them (44). Similar results were found in cabbage, spinach, celery, garland chrysanthermum, lily bulb, and taro (44). Only trace amounts of vitamin B12 (0.1 mcg/100 g of wet weight edible portion), which was estimated by subtracting the alkali-resistant factor from total vitamin B12, were found in broccoli, asparagus, Japanese butterbur, mung bean sprouts, tassa jute, and water shield (44). These vegetables may have the ability to take up vitamin B12 found in certain organic fertilizer."
"As bioavailability of the algal vitamin B12 is not clear in humans, my colleagues and I characterized corrinoid compounds to determine whether the dried purple and green lavers and eukaryotic microalgae (Chlorella sp. and Pleurochrysis carterae) used for human food supplements contain vitamin B12 or inactive corrinoids. My colleagues and I found that these edible algae contain a large amount of vitamin B12 without the presence of inactive corrinoids (54–57)."
Amazoniac
Member
https://www.researchgate.net/profile/Carmen_WheatleyWheatley [1,22] has described the vitamin as a ‘Scarlet Pimpernel’ for the resolution of inflammation
↳ A scarlet pimpernel for the resolution of inflammation? The role of supra-therapeutic doses of cobalamin, in the treatment of systemic inflammatory response syndrome (SIRS), sepsis, severe and septic or traumatic shock
↳ The return of the Scarlet Pimpernel: Cobalamin in inflammation II - Cobalamins can both selectively promote all three nitric oxide synthases (NOS), particularly iNOS and eNOS, and, as needed, selectively inhibit iNOS and nNOS
↳ Cobalamin in inflammation III - Glutathionylcobalamin and methylcobalamin/adenosylcobalamin coenzymes: The sword in the stone? How cobalamin may directly regulate the nitric oxide synthases
↳ The return of the Scarlet Pimpernel: Cobalamin in inflammation II - Cobalamins can both selectively promote all three nitric oxide synthases (NOS), particularly iNOS and eNOS, and, as needed, selectively inhibit iNOS and nNOS
↳ Cobalamin in inflammation III - Glutathionylcobalamin and methylcobalamin/adenosylcobalamin coenzymes: The sword in the stone? How cobalamin may directly regulate the nitric oxide synthases
It's such a shame that I didn't pay enough attention to B12. It's quite important and once the demands are increased by stress, unless the diet is providing plenty, it's likely that over time it becomes depleted.
I suspect that another reason for the elimination of animal proteins in Gerson's protocol during the initial period is to be able to normalize methyl and sulfur cycling with all nutrients that are directly involved. When this is resolved, some dairy can be reintroduced and it's then protective. If done too early, perhaps it just contributes to the mess. The ratio of micro to macronutrients needs to be higher when people are recovering.
@chrismturner89
Cobalamin is red, perhaps it's susceptible to visible light. Being bound to proteid might protect it from degradation, but I don't know if milk that's exposed to bright light in shelves has its content affected. On the previous post the pimps* commented that the "presence of hydroxocobalamin was not unexpected as it is the product of photolysis of the light-sensitive cobalamins [adenosyl, methyl, etc]".
*I don't know what pimpernel means, but I'm not going to find out because it's funnier this way, just like straw man. Please don't explain them to me, otherwise I'll cover my ears and make the arab ululatings.
It's also susceptible to the invisible part:
- https://www.tandfonline.com/doi/full/10.4161/derm.20013
"UVA radiation penetrates more deeply into the skin than UVB, and reaches not only epidermis, but also dermis with blood vessels affecting dermal dendritic cells, dermal fibroblasts, endothelial cells, mast cells, and granulocytes.80 UVA radiation is absorbed by pyridine nucleotides (NAD and NADP), riboflavins, porphyrins, pteridines, cobalamins and bilirubin.80 Porphyrins and riboflavins are photosensitizers. UVA effects are dominated by indirect DNA damage caused by reactive oxygen species such as singlet oxygen."
Out of curiosity:
- Nicotinamide adenine dinucleotide - Wikipedia
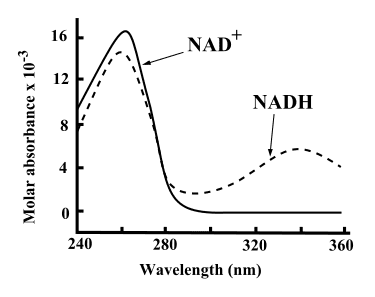
"Both NAD+ and NADH strongly absorb ultraviolet light because of the adenine. For example, peak absorption of NAD+ is at a wavelength of 259 nanometers (nm), with an extinction coefficient of 16,900 M−1cm−1. NADH also absorbs at higher wavelengths, with a second peak in UV absorption at 339 nm with an extinction coefficient of 6,220 M−1cm−1.[6] This difference in the ultraviolet absorption spectra between the oxidized and reduced forms of the coenzymes at higher wavelengths makes it simple to measure the conversion of one to another in enzyme assays – by measuring the amount of UV absorption at 340 nm using a spectrophotometer.[6]"

.
--
Four Forms of Vitamin B12 - Which one to take?
Last edited:
Amazoniac
Member
- Comparative Bioavailability and Utilization of Particular Forms of B12 Supplements With Potential to Mitigate B12-related Genetic Polymorphisms
"Animals store bioavailable vitamin B12 compounds in their milk, eggs, muscles and organs, and especially in the liver.11 AdCbl is the predominant B12 form found in meats, at 68%, with the rest occurring as OHCbl and MeCbl.12 MeCbl is the predominant form in milk and eggs."
"[..]a 2010 study assessed B12 status versus B12 intake by measuring homocysteine and methylmalonic acid and concluded: “In persons with normal absorption, our data indicate that an intake of 4–7 μg of vitamin B12/d is associated with an adequate vitamin B12 status, which suggests that the current RDA of 2.4 μg of vitamin B12/d might be inadequate for optimal biomarker status, even in a healthy population between 18 and 50 years of age.”16"
"Vitamin B12 occurs in foods bound in a protein matrix, from which it needs to be liberated during digestion, unlike B12 added as fortification. The bioavailability of foodderived B12 depends on adequate chewing and on the levels of stomach acid and proteolytic enzymes. After liberation from the food matrix, B12 binds to haptocorrin (HC), also called R factor, which is a protein secreted in the saliva and stomach fluids and which carries B12 along the gastrointestinal tract. Subsequently, proteolytic enzymes are needed to liberate B12 from HC to make it available for 2 distinct routes of absorption, either (1) binding to the intrinsic factor (IF) protein or (2) being taken into the gastrointestinal mucosa by diffusion. IF facilitates B12 absorption by the endocytosis route in the ileum, but it gets saturated at the level of 2 μg of B12 per meal."
"All conditions that involve impaired production of IF, such as autoimmune pernicious anemia or atrophic gastritis, and/or a compromised intestinal absorptive function, as in celiac disease, ulcerative colitis, Crohn’s disease, or tropical sprue, may greatly impair B12 absorption by endocytosis."
"Unlike vitamin B12 found in food, supplemental B12 is not bound to proteid; therefore, it readily binds to HC, and it is also available for direct absorption by diffusion. The supplement’s delivery system may be a sublingual lozenge, a liquid, or a capsule or tablet that is meant to open up in the stomach or lower intestinal tract. It is not clear if or how much absorption occurs by the oral mucosa route owing to inadequate studies comparing sublingual with encapsulated B12.3,4 The sublingual formulations may achieve partial absorption directly through the oral mucosa, but it is conceivable that part of the B12 may be bound by HC immediately in the saliva and then carried down to be absorbed in the GI tract by IF or by diffusion. B12 bioavailability from a nutritional supplement is not impaired in cases of low stomach acidity."
"All forms of B12 that are absorbed in the blood are transported by transcobalamin-I (TC-I) and transcobalamin- II (TC-II).5 One study observed that AdCbl seems to be the preferred form for binding to TC-II, whereas MeCbl is bound by both TC-II and TC-I.22 Because only TC-II delivers B12 inside cells, owing to specialized receptors, it appears that the AdCbl form of B12 may be delivered more efficiently to body cells than the MeCbl form."
"Two forms of B12, MeCbl and AdCbl, are recognized as active forms of B12 in human and animal physiology because they act as cofactors in important metabolic reactions. However, numerous studies have shown that those forms of B12 are not retained intact in their active form when they are ingested from foods or supplements because they go through intracellular metabolism.2,23,24"
"Numerous studies and reviews of B12 metabolism have shown that CNCbl, MeCbl, OHCbl, and AdCbl are reduced to the core cobalamin molecule inside the cytosol. It is important to note that the ligands specific to the ingested B12 form—methyl and adenosyl—are removed during that process and not used inside cells during the conversion of cobalamin to the 2 active forms of B12 (Figure 1).6,25-30 Activation of cobalamin occurs in very specific cellular environments; cobalamin is converted into MeCbl inside the cytosol and to AdCbl inside mitochondria. The final amounts and ratios of MeCbl and AdCbl produced do not depend on the initial form of B12 that had entered the cells.25 However, those amounts might vary based on cell type, specific cellular conditions, and genetic polymorphisms of those metabolic pathways."
"A cellular study has clarified that the methyl group brought inside cells by supplementation with MeCbl is not used in any methylation reactions and that supplementation with that form of B12 does not produce more methionine as compared with supplementation hydroxycobalamin.25"
"Another cellular study showed that the lysosomal reduction to cobalamin, when B12 is supplemented as AdCbl, was 67 times slower than the reduction of MeCbl to cobalamin. Thus, AdCbl supplementation may result in a slower synthesis of intracellular AdCbl and MeCbl compared with MeCbl supplementation.31"
"Intracellular synthesized SAMe derives its methyl component either from 5-methyl-tetrahydrofolate, with cobalamin acting as an intermediate carrier of the methyl group, or from intake of methionine, betaine, or choline. Thus, intracellular levels of SAMe are not influenced by the form of B12 ingested."
"It is clear that the form of B12 entering the body does not differentially influence the metabolite levels in any methylation reactions. However, the amount of vitamin B12 ingested at one time and its bioavailability, reflected by the portion converted to cobalamin inside cells, is relevant. Those factors can influence the extent to which 5-MTHF, available inside cells, will be used for methylation reactions and DNA synthesis.32,33"
"Inside the mitochondria, a portion of available cobalamin is converted to AdCbl, a cofactor for the conversion of methylmalonyl CoA (MMCoA) to Succinyl-CoA, which enters the Krebs cycle."
"All B12 forms [can be] converted to AdCbl, because they are all broken down to cobalamin first while the adenosyl group that is used to assemble AdCbl is synthesized from adenosine triphosphate inside the mitochondria.26,29 Consequently, if supplemental B12 is in the AdCbl form, it is unlikely that the total AdCbl produced inside the mitochondria would be higher compared with that derived from other supplemental B12 forms.6"
"Glutathionylcobalamin (GSHCbl) is an intermediate in cobalamin metabolism. GSHCbl is a newly proposed active form of B12, a cofactor affecting nitric oxide production, protection, and action in reactions associated with cell membranes.34,35 Those effects may have profound implications for vascular and immune health, but the results of those studies are preliminary.36-39"
"Supplementation with AdCbl has been shown to modulate the immune response by downregulating excess inflammatory processes that are mediated by inducible nitric oxide.37 That fact may explain why B12 supplementation has been shown to reduce the severity of autoimmune conditions, such as rheumatoid40 and atopic dermatitis.41 It is likely that all forms of B12 may have those effects, because they are all converted to intracellular GSHCbl."
"[..]a 2010 study assessed B12 status versus B12 intake by measuring homocysteine and methylmalonic acid and concluded: “In persons with normal absorption, our data indicate that an intake of 4–7 μg of vitamin B12/d is associated with an adequate vitamin B12 status, which suggests that the current RDA of 2.4 μg of vitamin B12/d might be inadequate for optimal biomarker status, even in a healthy population between 18 and 50 years of age.”16"
"Vitamin B12 occurs in foods bound in a protein matrix, from which it needs to be liberated during digestion, unlike B12 added as fortification. The bioavailability of foodderived B12 depends on adequate chewing and on the levels of stomach acid and proteolytic enzymes. After liberation from the food matrix, B12 binds to haptocorrin (HC), also called R factor, which is a protein secreted in the saliva and stomach fluids and which carries B12 along the gastrointestinal tract. Subsequently, proteolytic enzymes are needed to liberate B12 from HC to make it available for 2 distinct routes of absorption, either (1) binding to the intrinsic factor (IF) protein or (2) being taken into the gastrointestinal mucosa by diffusion. IF facilitates B12 absorption by the endocytosis route in the ileum, but it gets saturated at the level of 2 μg of B12 per meal."
"All conditions that involve impaired production of IF, such as autoimmune pernicious anemia or atrophic gastritis, and/or a compromised intestinal absorptive function, as in celiac disease, ulcerative colitis, Crohn’s disease, or tropical sprue, may greatly impair B12 absorption by endocytosis."
"Unlike vitamin B12 found in food, supplemental B12 is not bound to proteid; therefore, it readily binds to HC, and it is also available for direct absorption by diffusion. The supplement’s delivery system may be a sublingual lozenge, a liquid, or a capsule or tablet that is meant to open up in the stomach or lower intestinal tract. It is not clear if or how much absorption occurs by the oral mucosa route owing to inadequate studies comparing sublingual with encapsulated B12.3,4 The sublingual formulations may achieve partial absorption directly through the oral mucosa, but it is conceivable that part of the B12 may be bound by HC immediately in the saliva and then carried down to be absorbed in the GI tract by IF or by diffusion. B12 bioavailability from a nutritional supplement is not impaired in cases of low stomach acidity."
"All forms of B12 that are absorbed in the blood are transported by transcobalamin-I (TC-I) and transcobalamin- II (TC-II).5 One study observed that AdCbl seems to be the preferred form for binding to TC-II, whereas MeCbl is bound by both TC-II and TC-I.22 Because only TC-II delivers B12 inside cells, owing to specialized receptors, it appears that the AdCbl form of B12 may be delivered more efficiently to body cells than the MeCbl form."
"Two forms of B12, MeCbl and AdCbl, are recognized as active forms of B12 in human and animal physiology because they act as cofactors in important metabolic reactions. However, numerous studies have shown that those forms of B12 are not retained intact in their active form when they are ingested from foods or supplements because they go through intracellular metabolism.2,23,24"
"Numerous studies and reviews of B12 metabolism have shown that CNCbl, MeCbl, OHCbl, and AdCbl are reduced to the core cobalamin molecule inside the cytosol. It is important to note that the ligands specific to the ingested B12 form—methyl and adenosyl—are removed during that process and not used inside cells during the conversion of cobalamin to the 2 active forms of B12 (Figure 1).6,25-30 Activation of cobalamin occurs in very specific cellular environments; cobalamin is converted into MeCbl inside the cytosol and to AdCbl inside mitochondria. The final amounts and ratios of MeCbl and AdCbl produced do not depend on the initial form of B12 that had entered the cells.25 However, those amounts might vary based on cell type, specific cellular conditions, and genetic polymorphisms of those metabolic pathways."
"A cellular study has clarified that the methyl group brought inside cells by supplementation with MeCbl is not used in any methylation reactions and that supplementation with that form of B12 does not produce more methionine as compared with supplementation hydroxycobalamin.25"
"Another cellular study showed that the lysosomal reduction to cobalamin, when B12 is supplemented as AdCbl, was 67 times slower than the reduction of MeCbl to cobalamin. Thus, AdCbl supplementation may result in a slower synthesis of intracellular AdCbl and MeCbl compared with MeCbl supplementation.31"
"Intracellular synthesized SAMe derives its methyl component either from 5-methyl-tetrahydrofolate, with cobalamin acting as an intermediate carrier of the methyl group, or from intake of methionine, betaine, or choline. Thus, intracellular levels of SAMe are not influenced by the form of B12 ingested."
"It is clear that the form of B12 entering the body does not differentially influence the metabolite levels in any methylation reactions. However, the amount of vitamin B12 ingested at one time and its bioavailability, reflected by the portion converted to cobalamin inside cells, is relevant. Those factors can influence the extent to which 5-MTHF, available inside cells, will be used for methylation reactions and DNA synthesis.32,33"
"Inside the mitochondria, a portion of available cobalamin is converted to AdCbl, a cofactor for the conversion of methylmalonyl CoA (MMCoA) to Succinyl-CoA, which enters the Krebs cycle."
"All B12 forms [can be] converted to AdCbl, because they are all broken down to cobalamin first while the adenosyl group that is used to assemble AdCbl is synthesized from adenosine triphosphate inside the mitochondria.26,29 Consequently, if supplemental B12 is in the AdCbl form, it is unlikely that the total AdCbl produced inside the mitochondria would be higher compared with that derived from other supplemental B12 forms.6"
"Glutathionylcobalamin (GSHCbl) is an intermediate in cobalamin metabolism. GSHCbl is a newly proposed active form of B12, a cofactor affecting nitric oxide production, protection, and action in reactions associated with cell membranes.34,35 Those effects may have profound implications for vascular and immune health, but the results of those studies are preliminary.36-39"
[39] The gorilla link above.
."Supplementation with AdCbl has been shown to modulate the immune response by downregulating excess inflammatory processes that are mediated by inducible nitric oxide.37 That fact may explain why B12 supplementation has been shown to reduce the severity of autoimmune conditions, such as rheumatoid40 and atopic dermatitis.41 It is likely that all forms of B12 may have those effects, because they are all converted to intracellular GSHCbl."
For less details:
"All forms of B12—CNCbl, MeCbl, OHCbl, and AdCbl—seem to be absorbed with similar efficiency in the blood stream but differ in overall bioavailability, as reflected by their tissue retention rates. That fact may be due to different affinities for the blood-transport binding proteins, cell receptors for B12 uptake, and intracellular enzymes involved in their conversion to intracellular cobalamin. All of the B12 forms are reduced to the core cobalamin molecule inside the cytosol and then converted to the 2 active forms of B12—MeCbl and AdCbl—irrespective of the form of B12 ingested. It is important to understand that the conversions to active B12 forms do not employ the methyl or adenosyl ligand from supplemental MeCbl or AdCbl, respectively. The methyl group is derived from other molecules—5-MTHF, SAM-e, or betaine— while the adenosyl group is synthesized inside cells."
"As a result, the form of ingested B12 may influence how much cobalamin is produced inside cells but not how it is converted to MeCbl, AdCbl, or various active metabolites involved in methylation reactions. Genetics may affect the activity of enzymes involved in absorption, binding to B12 blood transport or intracellular proteins and/or B12 metabolism. However, no polymorphisms are analyzed through commercially available clinical tests that justify the use of any particular form(s) of B12."
"The current review shows that claims, such as “supplemental OHCbl delivers fewer methylating metabolites than supplemental MeCbl” are not scientifically substantiated. Supplemental OHCbl may deliver more, less, or the same amount of cobalamin inside cells as other B12 forms, thus resulting in the production of higher, lower, or equal amounts of intracellular MeCbl, respectively."
"Ingestion of CNCbl results in lower tissue retention of active vitamin B12 than the naturally occurring forms of B12, which may be particularly problematic in individuals with SNPs on B12 metabolic pathways. Researchers also have expressed concerns of potential cyanide accumulation in human tissues after long-term supplementation and/or intake from foods fortified with CNCbl. Thus, the CNCbl form of B12 seems to be an inferior choice despite its lower cost."
"One animal study compared the effects of supplementation with MeCbl versus CNCbl and showed that CNCbl urinary excretion that was 3 times higher than that of MeCbl. Although absorption in the blood of the 2 B12 forms was similar, the study found that MeCbl supplementation caused 13% more cobalamin to be stored in the liver than did CNCbl supplementation.7"
"Based on the considerations discussed in the current article, it is possible that individuals with particular SNPs [Scottish National Parties] affecting B12 assimilation might raise their B12 status more efficiently with 1 or more particular forms of vitamin B12. However, because those types of SNPs are not currently reported in commercial tests, individuals may require either a trial-and-error approach by supplementing with one particular form of B12 at a time, or they might simply use a supplement with a combination of all 3 naturally occurring forms of B12 that are commercially available for a better chance of achieving faster clinical results. That approach may or may not offset genetic polymorphisms involving B12 metabolism and related pathways. The injectable form of B12 hydroxocobalamin is a justifiable choice when high dose oral B12 is not successful. This administration route may overcome severe absorption impairments due to pathologies or SNPs.6"
@Blossom @Sheila
Very informative, thanks @Amazoniac.
SB4
Member
- Joined
- Sep 25, 2016
- Messages
- 288
@Amazoniac Good info. Going over my OAT I noticed my MMA was top of the reference range 2.3 (<2.3).
I am going to order B12 oil as I have tried high doses of different forms of oral and sublingual B12 without noticing much effect.
I am going to order B12 oil as I have tried high doses of different forms of oral and sublingual B12 without noticing much effect.
EMF Mitigation - Flush Niacin - Big 5 Minerals
Similar threads
- Replies
- 15
- Views
- 6K
- Replies
- 13
- Views
- 3K
- Replies
- 12
- Views
- 3K
- Replies
- 7
- Views
- 5K
- Replies
- 0
- Views
- 2K
- Replies
- 3
- Views
- 3K
- Replies
- 56
- Views
- 25K
