OP
stargazer1111
Member
- Joined
- Feb 16, 2017
- Messages
- 425
@stargazer1111, have you written out your history anywhere? Eg how you came to Peat and what health problems you had, progress etc. Looking at your post history I would be interested to hear it.
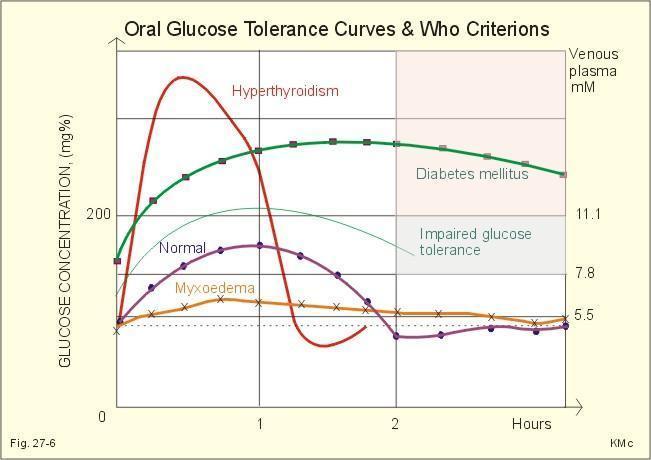
It is long and complicated for sure. I'm not entirely sure what my health history is because I didn't always see a doctor and wasn't always diagnosed. I have a history of hypoglycemia, especially in response to gluten. If I eat anything with gluten in it, my blood sugar is down in the 50s within 30 minutes of eating when it should be in the 140s at least.
But, I was never really diagnosed with anything other than abnormal thyroid function. I was in the early stages of hyperthyroidism back in 2010. My TSH was quite low but my T3 and T4 values were still normal. I ate a zero carb diet for several years trying to combat my hypoglycemia issues but finally added back in starch in 2016 because I felt so bad on zero carb. I did a moderate starch diet for a while but still felt rundown and not quite right. That is when I switched to a Peat-style diet. I had some symptoms of hyperthyroidism like the shakes, slightly elevated heart rate, and night sweats back in early 2016. But, I was still under the delusion that I had hypothyroidism because of all the crap I had read online. After doing a Peat-style diet for a couple of months, I noticed an elevated resting heart rate of about 100. After this, I started having tachycardia events where my pulse would shoot up near 180 and I would end up in the ER. The last time this happened, my heart beat so fast that I lost circulation and an ambulance had to pick me up. Each time I was there they checked my thyroid numbers and found that I was very hyperthyroid. Eventually, I had a thyroid scan done that showed overall inflammation and then an ultrasound that showed two nodules. They think the excessive amount of sugar probably exacerbated an underlying thyroid condition, especially since fructose increases the conversion of T4 to T3.
For the Peat diet, I consumed full-fat milk instead of skim because I hate skim milk. I drank orange juice, grape juice, blueberry juice, mexican sprite. I ate ice cream, the carrot salad, gelatin, and liver. I eventually ditched the liver and switched to a vitamin A supplement based on studies Haidut had posted about large doses being safe. But, understanding vitamin A chemistry so much better now, I realize how foolish that was.
Vitamin A did nothing to slow down my thyroid. I became more hyperthyroid while on the vitamin A, actually.
I had to add back in some PUFA and scale back the sugar. I don't eat zero sugar now. I just do a more balanced amount of sugar and starch and get about 10 grams of PUFA per day. The PUFA definitely help calm the thyroid down. If I get PUFA too low, my hyper symptoms come back.